The following is a transcript of the presentation video, edited for clarity.
It’s an honor to be here to share with you some ideas about treatment, and actually I’m to be giving you a little history about the treatment of dementia. Since it’s not that very long of a history of treatment, but a lot has been accomplished in the short amount of time. And I’m hoping that my remarks will by the end engender some ideas for new research areas and avenues proceeding from here on because I think the state of affairs is not where we want it to be at the moment and there’s a lot of room for growth and improvement.
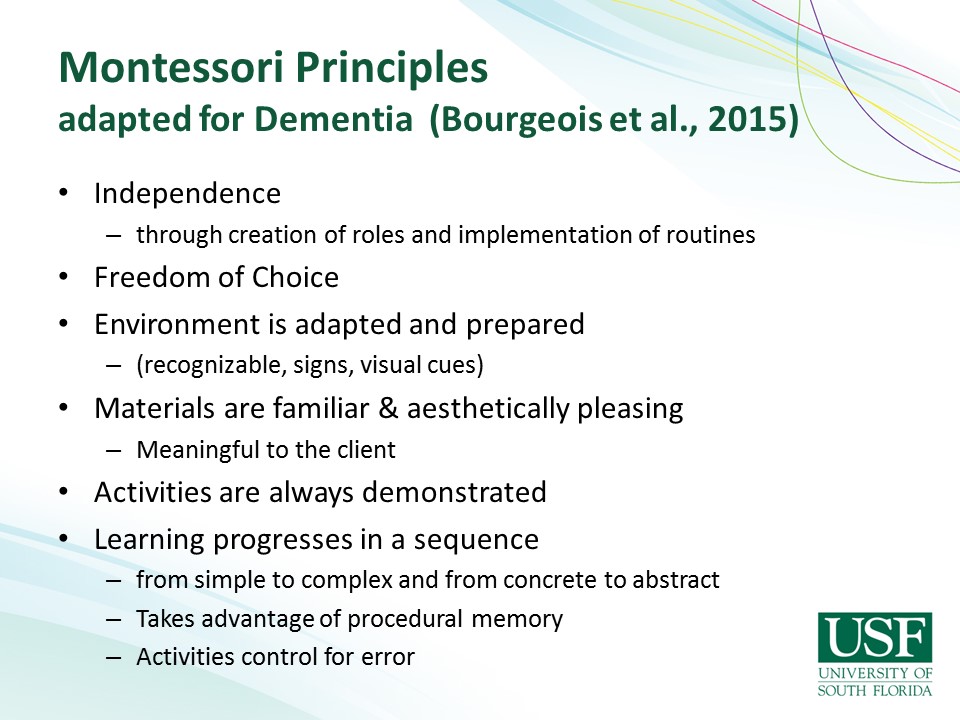
I’m sorry to admit that I forgot to put my disclosure slide in this. So I have to disclose that I work for the University of South Florida. I get a few royalties from the books that I’ve published. I have nonfinancial relationships with the Alzheimer’s Association because I review grants for them and also with the Association for Montessori Internationale which you’ll hear more about at the end of my talk.
Treatment of Dementia: A History
So where to start? I think we need to start where it started, at the beginning with Dr. Alzheimer’s who was first discovered this disorder, documented it with his patients, spend a little over a hundred years since the first reports of dementia were recorded. And it wasn’t really until the 1980s when dementia became apparent to us in our fields of speech pathology and audiology. It was then when we were first being referred patients who had this constellation of symptoms including memory loss for which people were complaining, “Surely there must be something you can do for my memory loss, it’s impairing my ability to have conversations with family and friends and really affecting the quality of my life.” And that’s where I entered this scene, I was fortunate to be right there at the beginning when we had no assessment tools, when we had no interventions, whatsoever and we sort to have to make it up as we were going along. I’m certainly indebted to Kathryn Bayles and her colleagues for being pioneers in documenting and developing the assessment tools that we needed along the way.
And over the past 30 years, we have done an excellent job through all of our various professions where we have been looking at and analyzing, assessing, documenting, figuring out what is this whole phenomenon of dementia. And we realize that it’s quite diverse. There are lots of variations, different and subtypes of dementia for our various ideologies, for various reasons. And in fact, you know, I wouldn’t be surprised if we would still uncover other types and variations as we go forward. It’s interesting that the DSM has decided that dementia now has such a bad rep. We have– People don’t want to be diagnosed with dementia. Everybody’s afraid of it, that they have decided to rename it. We’ll see how long it takes for people to adapt neurocognitive disorder, it’s a little more of words to say than dementia. But it’s certainly reflects the fact that a lot of work has been done to study and classify and understand the various symptoms and variations and symptoms of people with these cognitive disorders.
Along the way, people have been trying to figure out what the cause of these disorders are. There are obviously many, many different reasons and hypotheses about what causes it and how it’s related to normal aging and how it’s different from aging. The environmental influences, the immunological influences, all of the different types of genetic factors, there’s just some wide variety of reasons and theories of what causes dementia. And at this state, at this point in time, we, you know, we have our favorite theories but we’re really not, you know, quite sure entirely if we’re talking about one disease process or a lot of different disease processes. And it probably has going to end up that it is a lot of different things. There are some similarities, there’re some overarching conditions and factors that go into it but there are also a lot of differences and different reasons for it. It makes it difficult to study people with dementia, because of that it’s difficult to group them necessarily because of the different underlying reasons for the symptoms that they express.
Along with the way as well, as we’re trying to figure out the causes for these disorders, the medical profession has been trying to figure out how to treat it and because we have just hypothesis about different modes of operation, we have– they’ve only come up with the certain categories of medications and they’ve been quite disappointing. We still at this point have two major categories of memory enhancing medications, the cholinesterase inhibitors. For those of you who have experienced patients using these medications, you know, they have high expectations for the memory improvement and proving function and it’s disappointing that they don’t get very good effects. And for those people, who can take them, there are– there’re minimal effects. There’s certainly a large number of people who can not take them because of the side effects of these medications. Undoubtedly, there will be many more hypotheses about what medications might be effective. Back at when I graduated with my, oh when I got my doctorate in ’88, I was invited to Eli Lilly, the pharmaceutical company who was in the forefront of developing medications. And at that time in ’88, they had 23 different drugs under investigation. And we were told at that time, surely within five years, they’d have the medication, 30 years later, right? We still, they still are working at it and it’s going to be awhile.
In addition, because these memory enhancing medications have been disappointing, there’re still are behavior of symptoms that people with dementia exhibit that have necessitated some treatment approaches as well. And there have been a variety of antidepressants and other categories, especially antipsychotics that have been used and are continuing to be used with people with dementia to manage those negative symptoms of dementia.

And what is the effect at the current state? This is what our nursing homes look like. This is what our treatment failures are producing. We have a long way to go before this type of medical pharmacological treatment approach is going to create what we would rather be seeing which is more along these slides.

So there has been a real need for people to do non-pharmacological interventions and to explore those as well to see what other options there are if there aren’t some better ways to mediate the problems that coexist with the dementing conditions.
Cognitive Stimulation Approaches
But where we have a large amount of literature that is important to look at has been in the cognitive stimulation approaches and we’re going to review each of these domains, the cognitive stimulation, cognitive training and then cognitive interventions separately.
And we’re going to look at where this– the literature is in terms of the populations of people that these interventions have been done with. And it’s been interesting and useful that people have looked at these interventions starting with healthy aging adults just because people have not been sure what the relationship is with normal aging cognitive deficits and where to draw the line and where people convert from mild cognitive impairment to dementia. So there’s a whole continuum of cognitive functioning that these interventions or these approaches need to look at to see if there is any useful, usage for these in terms of improving situations.
Then the other point about why all of these interventions and all these research have– has come about is because of the fears we have of dementia and converting to dementia along the way if we have some mild– we’re finding problems as we age and other aging experiences. I’m sure most, everybody in this room is doing some kind of self-help pre-intervention for yourselves to try and stave off dementia or the effects of dementia. I know in my household, we do an awful lot of crossword puzzles and Sudoku because we hope that that’s going to prevent a cognitive impairment later on.
But do these things work? When I do workshops for people, older adults who come and want to learn about memory strategies, the first thing they’re asking me is, “If I do all these crossword puzzles, and I do all these Sudoku and all those stuff, is that going to help me? Is that going to prevent dementia?” And sadly, we don’t have the answers about it. There are a lot of studies out there. The evidence is accumulating, it’s promising, but it’s not definitive.
Some of the other things that the stimulation approaches include are the social activity interventions, so the idea that maybe, if we’re socially active and engaged, that will help maintain our cognitive functioning. A lot of studies have been done on that, some of them are longitudinal. And it’s interesting that what people measure on in a lot these studies are very specific things like delayed word recall, task that really are not reflective of what we do in everyday in life, but they’re very impairment-based, structure types of things. These studies are showing a variety of benefits, variety of things that people measure but you need to ask yourself what is it they’re measuring, what is that have to do with everyday functioning and– and look at that critically.
We also and as we heard– learn this morning have– or considering that social activity and social engagement with people may be related to hearing loss or vice versa and we’re still trying to figure that out as well. Certainly, if people are not hearing well and it’s difficult and challenging and it’s a lot of work to hear what people are saying, they’re obviously are not going to want, engage in social activities.
We’re learning that exercise may be even better than social engagement by itself and there’ve been studies that are showing that’s in exercise in addition to social activity. So walking and talking, going walking with your friends so you’re talking at the same time may have better effects on cognitive measures as well. But the word is still out on how much exercise you need, what type, frequency of the exercise, intensity it needs to be, all of that is there’s a lot of studies still ongoing to try and tease out all these variables. It’s likely to end up that it’s going to be very individual specific in certain groups and certain types of people will need different dosages of exercise to have effects.
And also video games and other kinds of stimulating activities that go beyond the social activity and exercising of quite a few studies on whether using the Wii games or the Nintendo or all of these computer type things are having effects. There are some evidence on some of the measures that they can show effects, but then again, how well that translates to everyday functioning is not clear.
The studies in cognitive training, so specifically looking and targeting specific cognitive skills have been done with healthy older adults, a lot of them have been done and there’ve been quite a few meta-analysis and systematic reviews of that and the types of trainings that they’ve looked at are what I term internal memory strategies, things that require a lot of cognitive effort to use and practice, things like using mnemonic and name-face associations, imagery or of those kinds of things. But they’re showing that average normally aging people who use these kinds of strategies in fact can benefit from them especially when people start them when they’re younger, when the training that’s done on these types of strategies are done in groups so that there are added benefits of having other people who are in your same situation, experiencing the same fears and losses or cognitive decline that you are to share and to do these things with. And when these sessions, the actual training things, are relatively short, not long protective things.
The most famous of studies and the most well-known is the Active Study where they’ve had almost 3,000 participants over many years, studying four different groups of people, randomized to these different groups focusing either on memory specifically in different types of memory strategies or inductive reasoning and a lot of this stuff is done either paper and pencil task or computer programs. A third group, speed of processing, so and this is done on the computer doing visual search types of games and then with the control group comparison. And they’ve shown in this study with all of these participants that they were able to measure differences, improvements on some standardized cognitive measures. And some of these effects maintained for five years. But when they studied and asked them about their quality of life or their possible impact it have on their activities of daily living, the results are not that great. They’re much more modest.
So that study and all of the other related ones generally show that healthy aging adults do benefit from learning memory strategies, from incorporating that. But there really needs to be more focus on helping people become more aware of what memory is and how memory is used and how we incorporate memory strategies and memory supports within our daily lives.
Every single one of you in this room uses multiple memory strategies every single day. All of you have cell phones, you have planners, you have calendars, you have– what, you know, I could go on and on. You use them everyday and you would not be able to be here and function in your daily lives without them. And I think one of the really important things that the group instruction approach for doing memory strategies training with healthy older adults and people with mild cognitive impairment is to share with them that this is a normal everyday activity. This is something we all need and use, sometimes without our own awareness of it but we need it to be able to get through our busy lives and all of that the information overload and stimulation that is in our everyday lives. So, but people that come to these groups and when you assess what they know about memory and memory strategies is it’s pretty, pretty low. They’re not sure of what’s going on. They just know that their memory is impaired, something is different. And in spite of successful implementation or use of strategies, there still is a lot of negative belief or negative self-efficacy regarding memory. People go through, successfully go through memory strategies courses and demonstrate marked increase use of memory strategies and yet when they’re asked, they still think they’re not doing well enough, it’s not good enough. They still forget that occasional word or they still have that, they forget that item at the grocery store. And that little lapses that they have become magnified and we need to work on helping– finding ways to help them be more realistic and more aware that the strategies are helping them. And also work on their anxiety. In spite of these positive results of these studies, people still have anxiety about dementia. They still fear that even if they do all these things, it’s still not enough.
A large body of literature is now been amassed about memory interventions, cognitive interventions for people with mild cognitive impairment. The types of studies are varied. The types of interventions, the types of skills and things that people work on are different. But largely, a lot of the cognitive training that’s been done with people with mild cognitive impairment has been computerized.
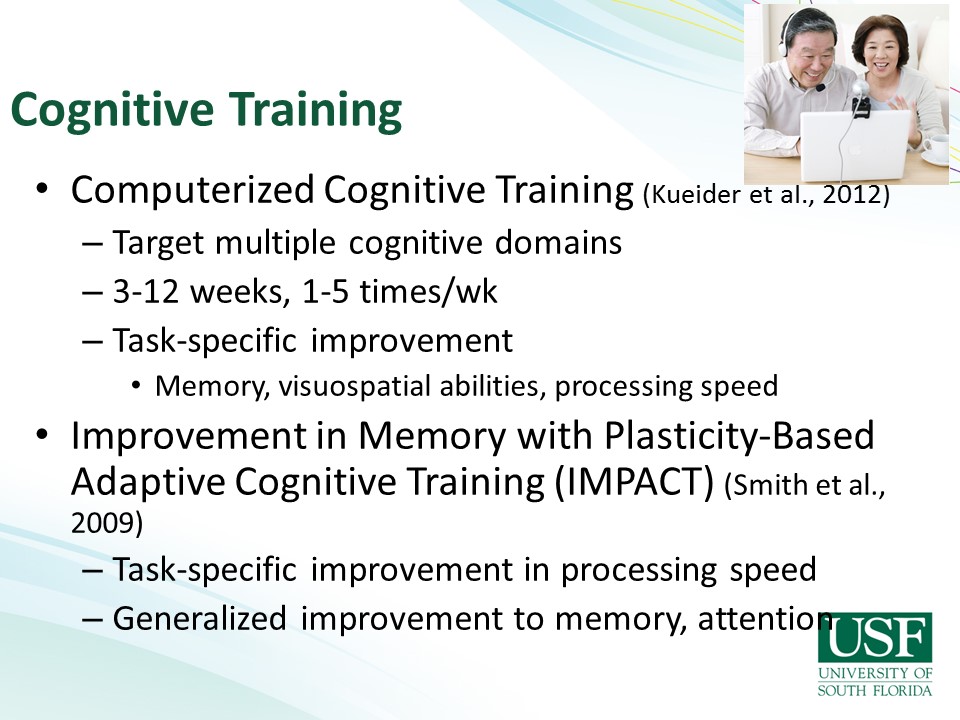
It’s a big literature-based on computerized cognitive training. And it’s interesting that people come to these memory strategies classes and also ask about that which memory game, which computer game, which computer program should I get? I wish I had stock in Lumosity. How many of you do the Lumosity? You know, they’re very clever. They have really wonderful marketing strategy, they really hook people in with their– the way they reinforce and motivate you to go to the next level and keep going and improving your memory even more. And what’s interesting about this literature is that people who enjoy doing computer games and enjoy this really believe that it’s making a difference and it’s helping. And some of these studies can measure specific changes on standardized measures and specific cognitive domains. However, there again is limited generalization or use of this information in their everyday life. And you just need to stop and think about what it is they’re doing with these– in these computer programs. These are repetitive tasks that are basically non-functional and we might like to believe that we are changing the brain somehow by doing that and there have been some people who in some studies where they’ve actually measured some brain functioning and shown some changes in brain functioning after working on computer games. But the reality is that doesn’t last. It’s temporary and you would have to be continually doing this all the time for– to make a difference and then, but that’s only if you enjoy it. If you don’t enjoy it, you’re not going to stick with it, you’re not going to do it and it won’t have the impact that you want.
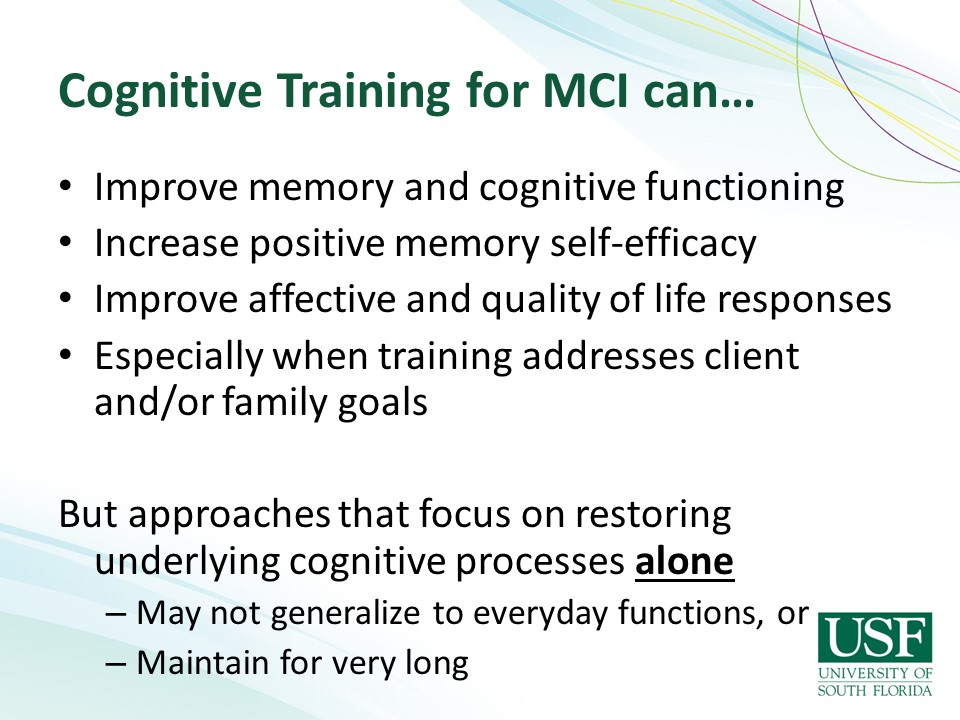
The other point that is important to make about these kinds of, this kind of cognitive training, computerized types of things is that the training– people get better at doing the task that they practice. And so if they’re practicing on the computer screen, you know, wiping out little dots or whatever it is that they’re doing or connecting dots, they’re going to get better at that. And it’s not going to generalize to anything useful in their everyday life. So we need to be cautious about it and to investigate it more and figure out better ways or better types of computer programs that might be more functional so that we can have people practicing things that make a difference in their everyday life.
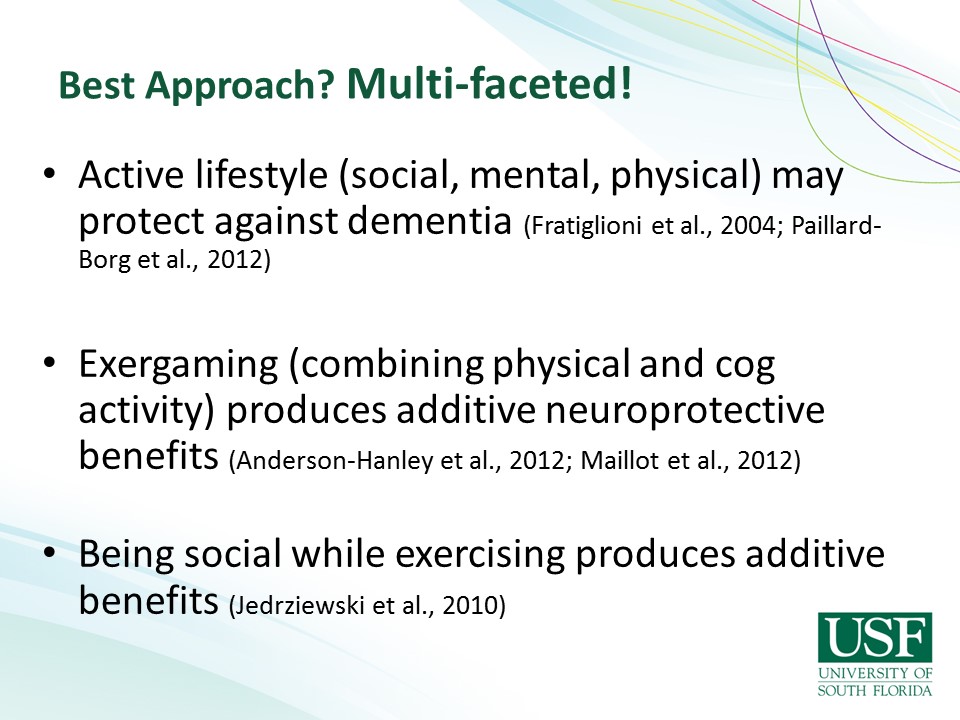
So in general, the cognitive training literature basically suggests that, and the cognitive stimulation, cognitive training literature suggests that there is not one single thing that has the evidence to support its use in terms of changing cognition, improving it or preventing dementia, the prevention piece is not there yet. And it’s likely to be a multifactorial thing that doing a variety of stimulating activities or training things or some memory supportive things will be helpful. But the word is still out on that.
Cognitive Interventions
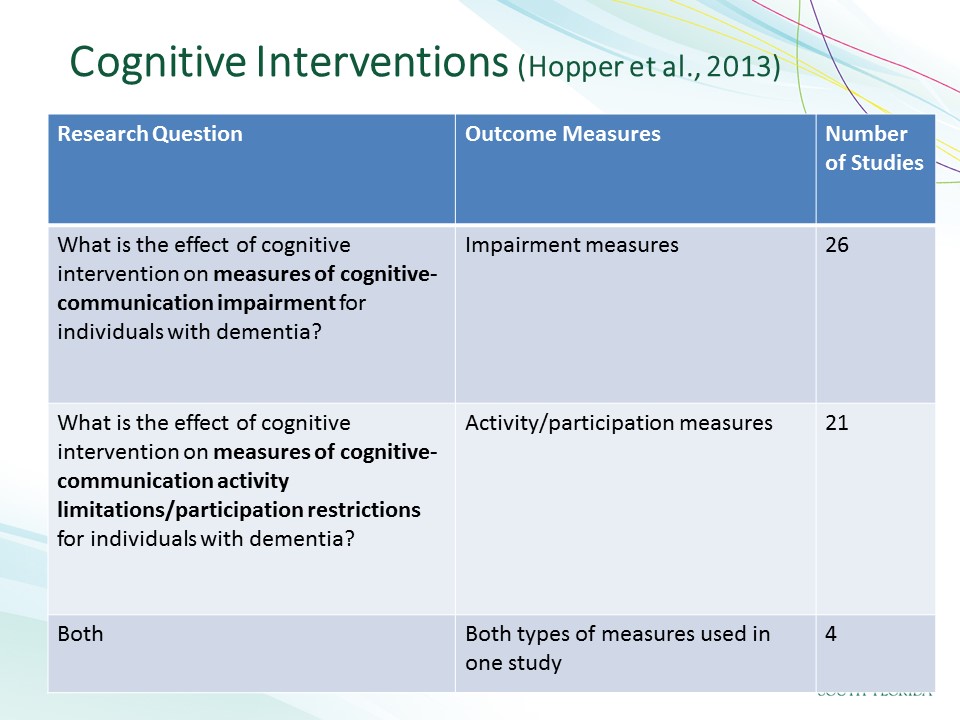
And I would like to switch to the cognitive interventions. So interventions that are targeted specifically to behaviors that are impaired, not the underlying cognitive function but the behaviors that are associated with the cognitive functions, and interventions that help improve these functioning. My colleagues, Tammy Hopper and a whole long list of others who with the assistance our folks at ASHA, did a systematic review of cognitive interventions. We were very interested in looking at what impairment-based measures people were using in these studies to look at what underlying changes there were in the cognitive processes, but also what changes and functioning in the activity and participation types of measures people were using. And so we found a large literature from which we had specific criteria that narrowed it down to the studies that we evaluated.
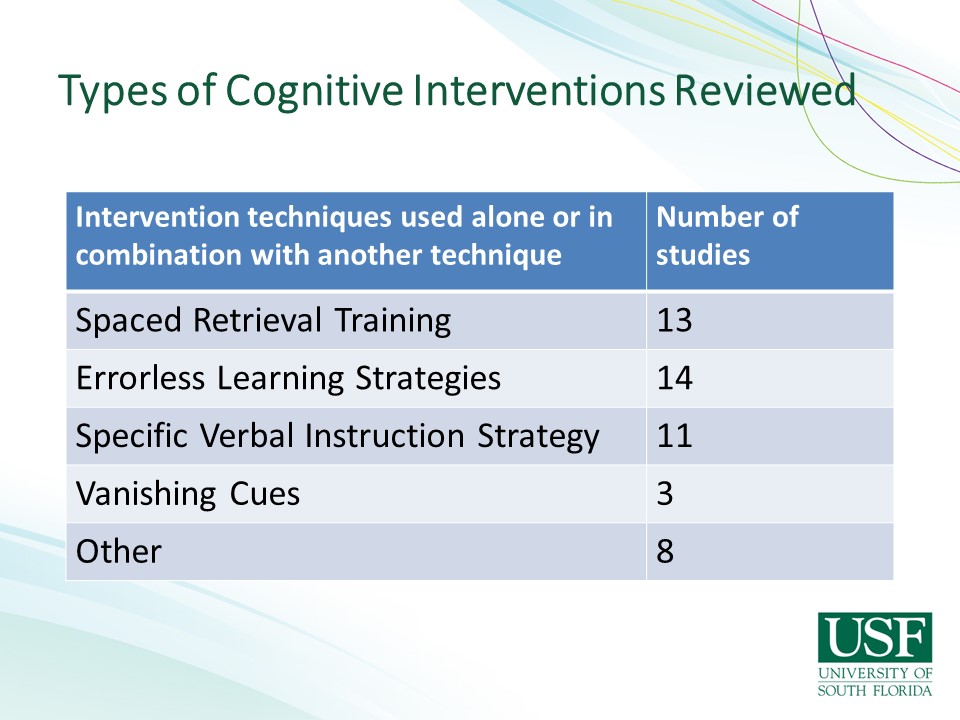
But what we were looking for were studies– interventions, training, things that would actually change functional behavior in people. And there are quite a few training approaches out there that have significant amount of evidence behind them now and these are the ones that we reviewed in this review and I’ll go over them individually, but spaced retrieval training and errorless learning strategies are the two predominant ones at the moment. There are a fair number of specific verbal learning strategies which it was actually surprising not to find more verbal learning strategies and vanishing cues is another type of a verbal strategy within our field because what we do is verbal practice and training, a lot of or all of our communication-base interventions are these verbal approaches. But I’m sure a lot of the studies in that regard possibly are in the category that we didn’t review for various reasons.
But let me talk about spaced retrieval training. And this approach is designed to strengthen conceptual associations by repeatedly activating a stimulus and response pair. And it gradually, having the person practice retrieving information, repeating it verbally, over increasing, expanding intervals. What this does, it has the person essentially practice remembering a specific piece of information for longer and longer periods of time. And there have been many, many studies done of spaced retrieval and what we find is that when someone has an opportunity to practice and retrieve information in a structured way in a training paradigm, that once they can hold on to information for up to five minutes before they’re asked and can retrieve it again successfully, when they get to a five-minute period of time that they can hold on to the information, then we believe it’s been moved into long term memory and then 24 hours later, you ask the person a question and they still remember it. And over and over, many, many studies with various types of behaviors and targets for what they’re remembering have demonstrated that people with dementia, all stages and severities of dementia with the structured type of training do in fact learn new information, the actual one information that’s relevant to their daily functioning or they can improve a strategy for using a memory book, for instance, or remembering to use a calendar or some other kind of a strategy and other types of functional everyday behaviors.
These types of activities have been done not only with people with dementia, we’ve done work in spaced retrieval with people with traumatic brain injury, with cognitive deficits for that. We’ve done spaced retrieval over the telephone because it’s a verbal strategy. We’ve done it in a variety of situations and a doctoral student in just did a beautiful study demonstrating the use of spaced retrieval, teaching people with severe dementia in nursing homes who have dysphagia to use a cue card for safe swallowing techniques. And people with severe dementia who– people otherwise would have thought it could not learn anything, through the use of this training strategy, in fact, could learn relatively easily to follow the steps, multiple steps for safe swallowing strategies and avoid the diet modifications that were being recommended for their dysphagia, so a variety of functional, everyday behaviors that– modifiable through spaced retrieval training.
The second training strategy that’s gone a lot of research done on it is errorless learning. Errorless learning is a technique for practicing information with a person that prevents them from making a mistake. So instead of what are gold standard in communication disorders is to give somebody a prompt and then wait for them, give them count to five or whatever to see what response they come up with, it’s the reverse of that. Instead of doing that, you– when you give them time to come with an answer, it could be the wrong answer and therefore, you are helping them retrieve errors which makes it more difficult for them to eventually learn that information that you want them to learn. So if you start with an errorless procedure and you say, my name is Michelle. What is my name? My name is Michelle. What is my name? And Michelle is my name. And they are repeating the information without an error, then you gradually increase the interval that they’re holding on to it and there’s variety of procedures for doing this but it also shows that this type of an errorless procedure allows people to learn information, factual information and also learn procedural problem solving task as well, very effective.
The third strategy is a verbal strategy, verbal instruction strategy using prompts, verbal prompts. It’s a variety of studies that have done, that have shown that you can successfully prompt the people verbally through tasks. They can learn their tooth brushing routine or whatever it is that they need to do in daily life to function appropriately.
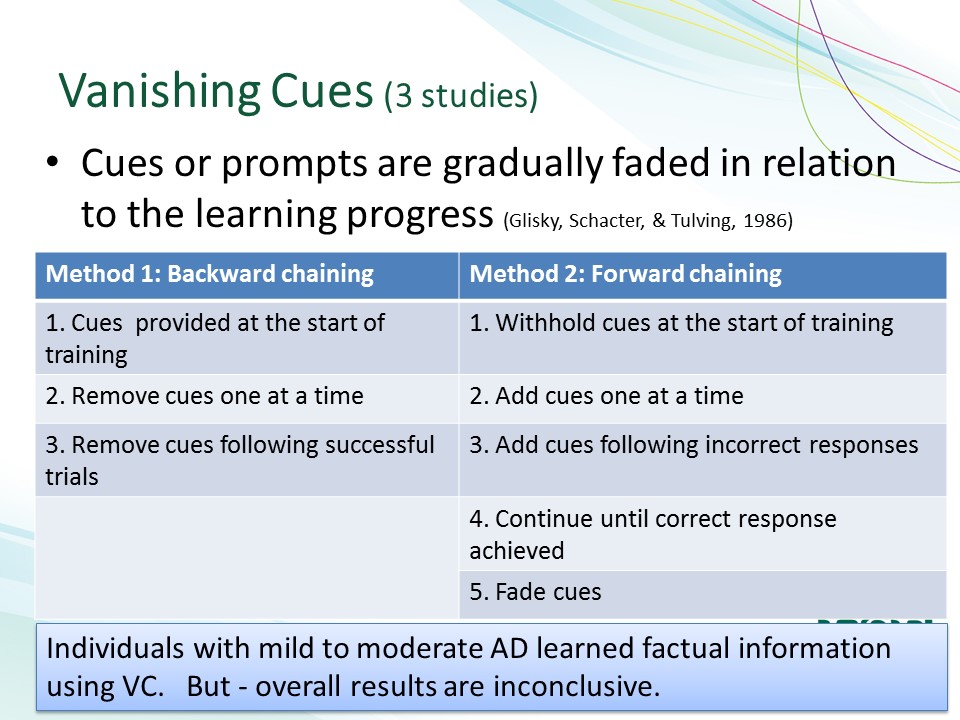
As well as a vanishing cue technique. We have several studies on that where the types of cues you give in one procedure of vanishing cues, you start with an intense cue and you gradually withdraw the intensity of the cues or you start with a minor, minimal cue and you build up as the person needs more cues. These types of cuing strategies also have been to shown to work quite effectively for functional task and behaviors that people need.
Other interventions that we’ve reviewed, there were fewer of them in our review included memory books and wallets.
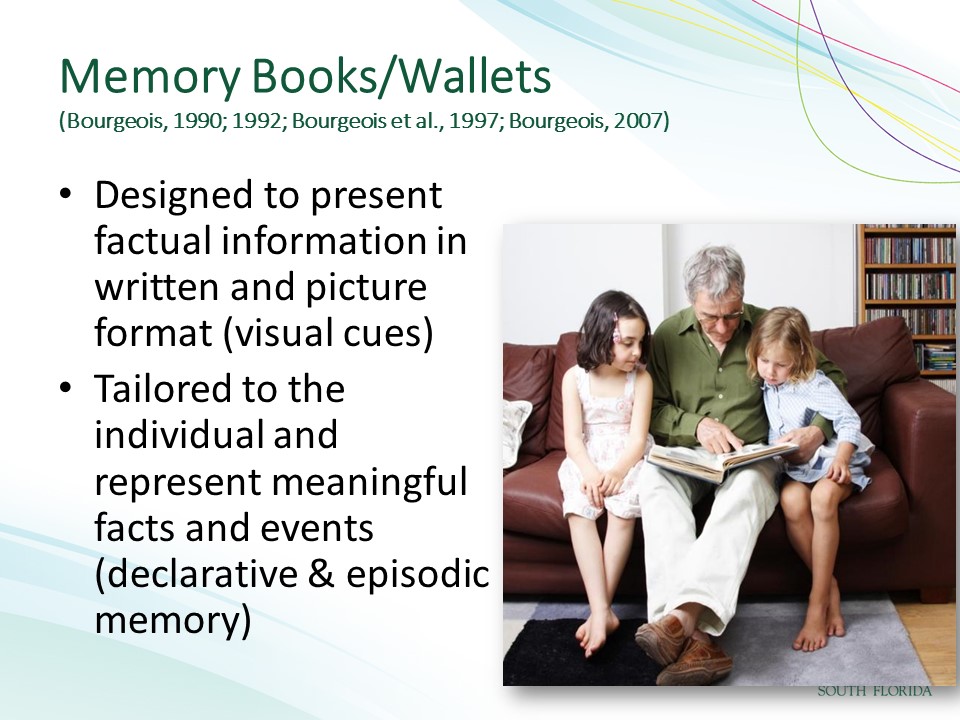
So my work over the years has been to show that providing visual cues in the form of pictures and text allow the person to read the text out loud and that triggers related memories and enables the person to function in conversation, have satisfying conversations.
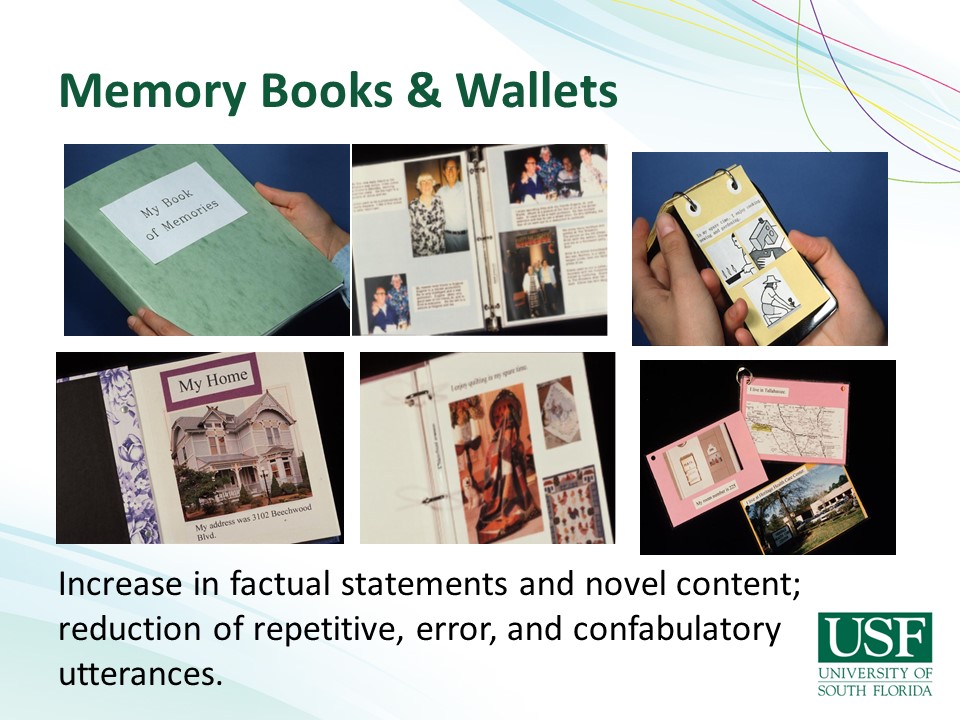
And over the years and all of the studies that I have done, variations of this approach with different severities of dementia, different types of memory books and wallets have shown that people, number one, have– people with dementia have preserved reading ability all the way till the very end of life because it’s an over learned behavior, it’s not necessarily and it’s over learned and automatic, it’s not a conscious behavior. And they can read as long as the sensory changes are attended to. So if they can’t read to the smaller print, you enlarge the size of the print until they can read it and that the information that you are asking them to talk about using these visual supports is personally relevant to them, that it’s their meaningful life history or their family or the topics of conversation that they want to be conversing about. When you have this kind of visual cue, the negative or the non-productive behaviors that people engage in without support in this fashion, the other things go away. So confabulatory behaviors go away, repetitive behaviors go away, making errors in what they’re saying go away. So this has been a very important discovery I guess of these types of interventions to show just how important visual cues are.
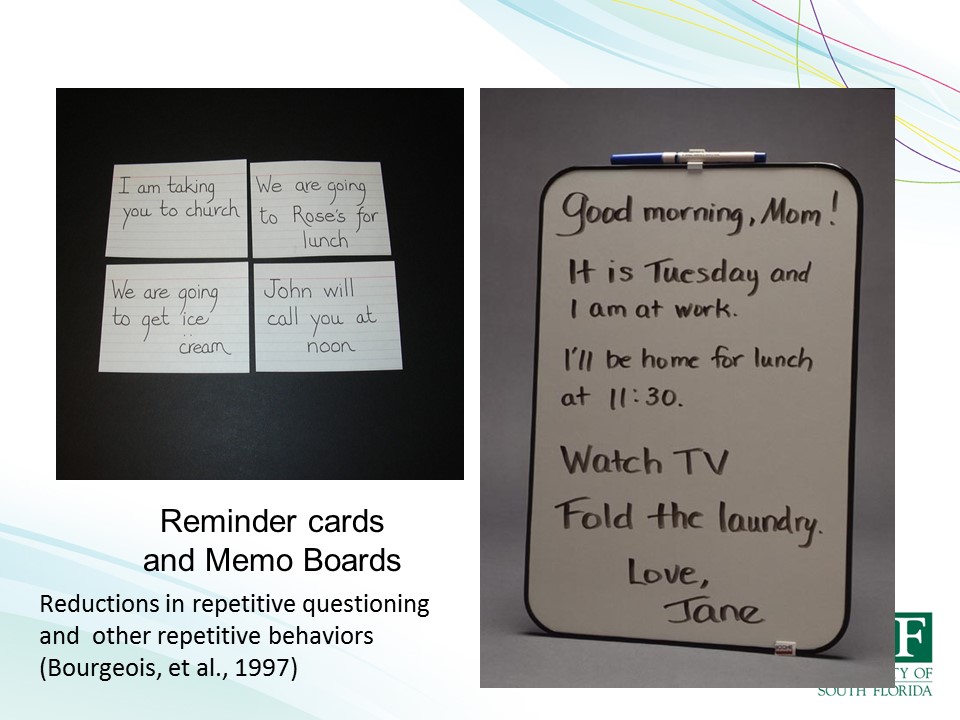
After showing that conversations can be improved, I was fortunate enough to discover along the way that a variety of behaviors can be modified with visual cues. Everything from the repetitive verbalizations and questioning that people with dementia have to a whole variety of anxiety-related behaviors and whatever by having written information that addresses the specific problem or anxiety that they’re having.
This has then expanded on to using visual cues for other purposes. The question, can people with dementia maintain their life long roles that they may have always held in life. If they were a parent, if they were a teacher, can they still engage in those kinds of roles in life if you give them visual supports? One study that my colleagues and I did was to show that people with dementia could teach children to make a recipe and make banana pudding following a visual memory, a visual recipe book, booklet. And measuring the language that they said during this task and comparing it to the language of age matched non-demented elder people doing the same task, we demonstrated that people with dementia could do this equally well, that the language that they said using these booklets and the instructions they gave and the reinforcement they gave to the children was identical to what the normal aging non-demented elders were doing. The only difference in the study between the two groups was that the people with dementia were a little slower, it took them a little longer, they took more time to do the recipes but all of the qualitative data, language data was proportionately the same. So it’s demonstrated that, that language is there, it needs to be cued and these kinds of visual supports can do that.
Visual cues are I think one of the major non-pharmacological treatment approaches that we need to be using with people with dementia in pair with some of our structured training approaches like spaced retrieval, errorless learning, vanishing cues, all of those structured approaches. And if we use those, we can modify and change a lot of the functional problem behaviors that people with dementia are facing.
But visual cues aren’t the only sensory cue that we should be addressing. We also need to address auditory cues. And years ago, Catherine Palmer, my audiology friends and I did a study putting hearing aids on people with dementia to see if any of the problem behaviors that we hypothesized were related to diminished hearing could be alleviated by improving their hearing through a hearing aid. And in fact, we demonstrated that in caregivers, the family members who complain of the repetitive verbalizations, the searching and pacing behaviors of people, hearing things that weren’t there, all of these problem behaviors that we hypothesize were related to hearing and they took data on. Once we had fitted the persons with the hearing aid and they wore those hearing aids, all of those behaviors diminished. Demonstrating the fact that having an improved auditory signal helps these folks with the types of behaviors that are related to their cognitive impairment.
Where Do We Go From Here?
So where do we go from here? So there’s a substantial body of literature in all of these different domains to demonstrate that non-pharmacological behavioral treatments for the cognitive problems of dementia are effective and are useful. And I would like to propose that we can use this literature, this evidence and go forward for sharing with people before they have a diagnosis of dementia that there are lots of things of people that can do to hopefully prevent or at least slow down or to compensate for the types of deficits that they are experiencing due to normal aging or mild cognitive impairment. We can suggest and encourage people to do cognitive stimulation types of things and even training types of things then that might be helpful for them. In the early stages of dementia, there is a lot of evidence that there are many effective treatment approaches for training people with the specific problem behaviors that they are experiencing through intervention approaches like spaced retrieval, visual cues, hearing aids that help people in those stages of dementia to function and to have a better quality of life.

But what do we do later on? Do we have this impression that once you get to a certain point in the dementia trajectory that it’s hopeless or eventually going to lose everything. And I would like to say that I don’t think this is inevitable. I don’t think even though I’ve spent the past 30 years of my life working in nursing homes generating all this evidence for the effectiveness of intervention approaches that we are using it yet. This is still going on and I think as we’re learning that there are barriers to using these approaches in our facility, our clinicians out there are not necessarily using a lot of these strategies or they’re coming up against people who are not wanting them to or are thinking that people with dementia are not capable of these approaches that we need to stop and think for a minute and maybe reflect on how we might overcome this challenge.

We know the evidence, the evidence is there, it works. How do we get these procedures, these methods implemented in the facilities where we need to? How can we change this which is what we see still to this? Is this not what we would hope our nursing homes would look like? What our community programs would look like? What we want in the near future, I’m getting close to retirement age, I’m looking ahead to when I’m in one of these facilities myself. This is what I want it to look like. I want to have fun, I want to enjoy my life, I want to have a quality life, meaningful. I think what we need do is stop and say, are all of these assessment tools and all of these things that we spent all of these time developing, is it– I mean, it’s been good, it’s great we’ve learned a lot but it’s not getting us where we need to be.
We need to stop and say, from the other direction, what’s meaningful? How do we get the type of life that we want to happen? And I think we need to say and we needed to ask our self, what are the components of a meaningful life? What are the ultimate objectives? What are the goals we have for ourselves, for our family members, for the people that we’re working with? And if you just think about what the components of a quality life are, you know, they’re very fundamental things.
First of all, food and shelter, I think we do that pretty well, you know, we’re pretty good at making sure there are– we have plenty of facilities everywhere around. We’re really good at the food thing, right? Speech pathologists in every nursing home do swallowing stuff galore, almost exclusively. You know, we’re focused on that so we do that that well. But let’s look also at some of the other things that we need to make sure are there for people, someone to love and to talk to and someone who loves you back. Isn’t that a fundamental need? Isn’t that a fundamental quality of life necessity? Something meaningful to do. We are all really active, busy people. Imagine if you, all of the sudden, had a time warp and right now, turned 80 and we’re in a facility. You’d be– You’d still revved up to be doing things and going some place and doing stuff and you’d want things to do that were meaningful. We’d put people in these facilities and have nothing for them to do or things that are not related to anything they like or would want to do. We need to think about and ask people what is meaningful to them. What would you like to be doing? If you have something meaningful to do, then there’s a reason to get up in the morning. I think, you know, we should be measuring depression in these, in facilities and measuring how we can change the depression and negative affect related to what types of activities and meaningful activities people have. And another component I think that we don’t usually think about but I think is it really, really important is be feeling useful in part of your community, having a role in your community, feeling appreciated for your contributions. I mean all of us now in our work, more or less, we are appreciated for what we do, we– we certainly, we get paid for what we do. So that’s one form of recognition but, you know, when our clients thank us, when, you know, we see change us in families where we have satisfaction that we’re doing a good job and we’re doing something meaningful. When people go to one term care and they o not have anything to do, they don’t have a role to play, they don’t feel part of the community, they feel disconnected and I think that contributes to despair of nursing homes.
So what I’m here today to do in the end is just to try and light a fire and spark some interest and changing the way we think about what we do. We have a long history of assessing people, figuring out what’s wrong with them, although in recent years, we’ve also added assessing what they still can do and figuring out both things. But the objective of that isn’t figure out a treatment to fix some, fix the things that are wrong with them. That approach I think is what is creating a lot of unnecessary and meaningless interventions or lack of interventions that people aren’t doing cognitive interventions in nursing home and just doing swallowing is because they’re not making the connection about what would be meaningful and useful. So I think and this approach is clinician focused. I’ve been telling my students that I needed them to change their terminology. Instead of saying, “I’m assessing my person and coming up with goals for them.” I think we need to be asking our clients what they want and figuring out where they want to be going and doing and figuring our goals with them instead and having a patient-centered approach. I think this is going to require flipping a rehab model. I think we need to get away from starting with assessment and ending with meaningless treatments.
And I think to do this, we need to start by saying what we do for assessment at the beginning is learn who our patients are, what they want, what’s meaningful to them, what they want to be doing, who they want to be communicating with, and what the barriers are to doing them.
Then we can tailor our assessment to figure out what we need to do in treatment to get them there, to get them what they want to be doing. And that will help create patient-centered goals that are going to lead to meaningful outcomes that are going to be very important for being able to do what we are now mandated to do.
So that with the change in the healthcare, and the Affordable Healthcare Act and this new focus on figuring out what the patient wants and having a patient-centered care approach and having the patients report the success and outcomes of our interventions. It’s imperative to me, I don’t think there’s any other way around it. We need to be asking them what they need and want and figuring out ways to help them achieve that.
Luckily, you know, the changes at the federal level coming along with money to develop the assessment tools and things to help us with that, these are some excellent websites for looking at the things that are under development and are they being ruled out.
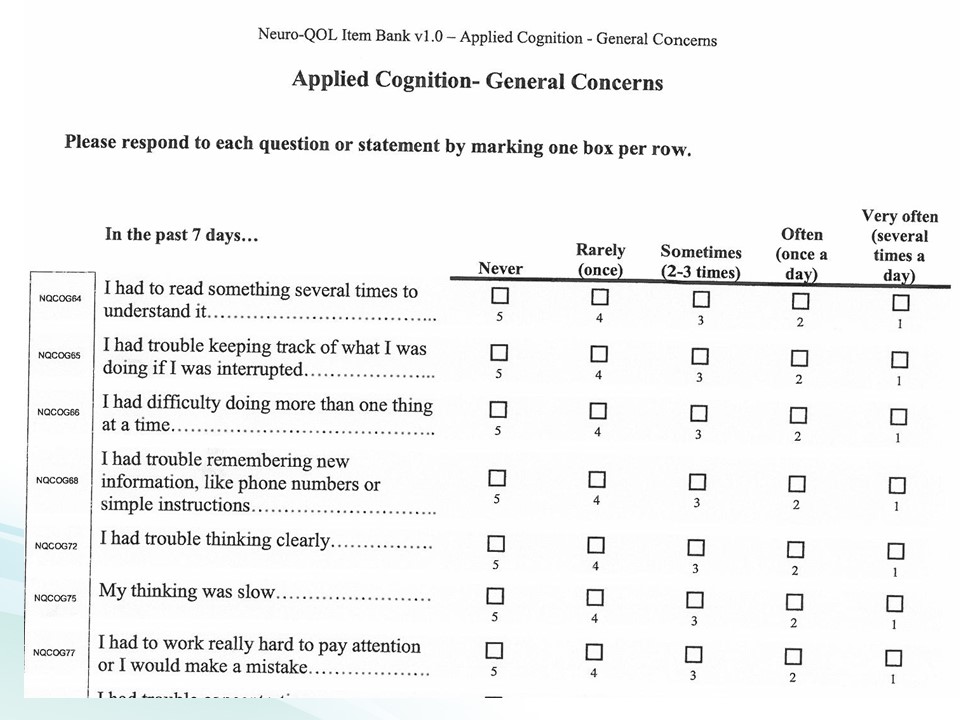
These are some examples. It’s very encouraging to see the functional nature of the questions. This is not the underlying cognitive process, this is the actual application of cognitive processes to functional behavior. This is general concerns.
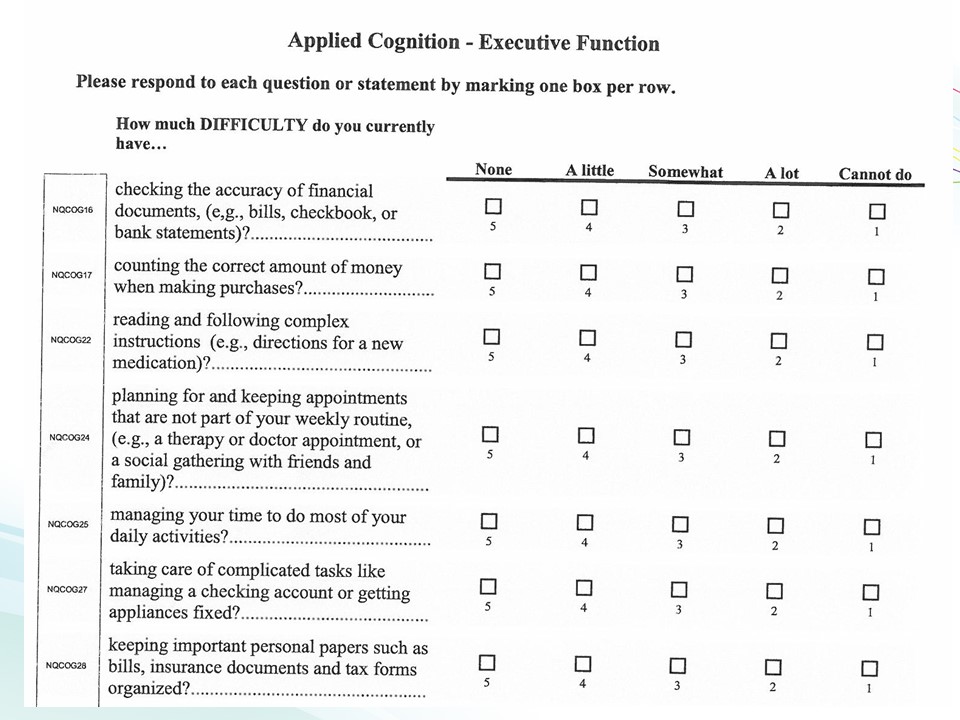
There’s executive function, you know, checking the accuracy of your checkbook and actual behaviors and things that require executive functioning are the things we’re measuring and making sure we can make changes in.
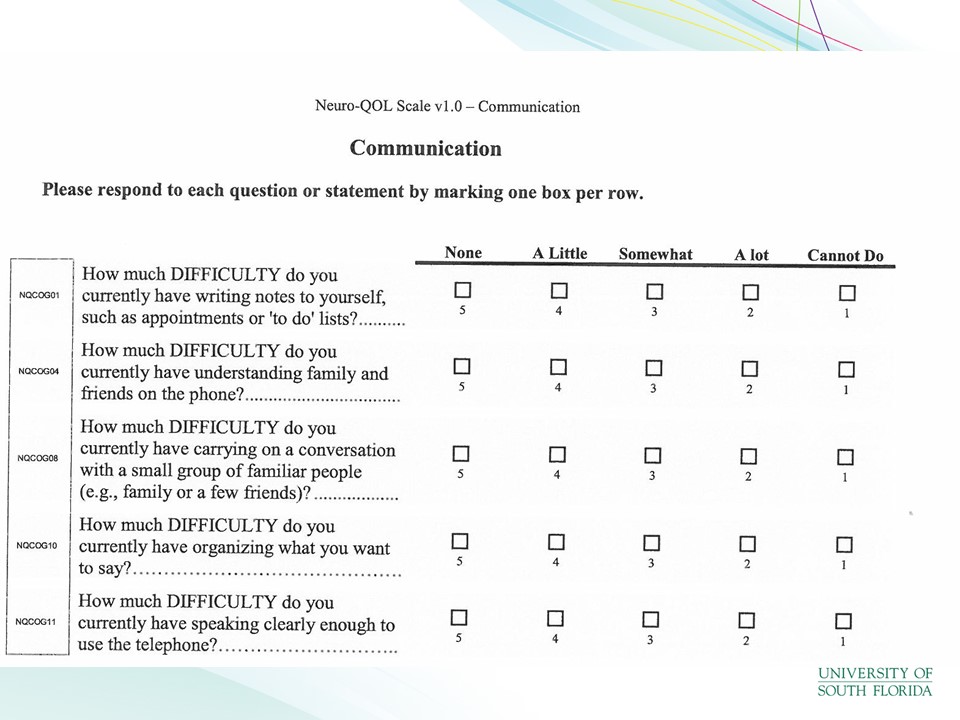
Communication, and these are similar to things on the ASHA facts and some of the things, over the years we’ve been playing around with this and trying to get this going. And I think we’re, you know, we need to do it now. We have to really get down to business and change the way we are assessing and looking at these things.
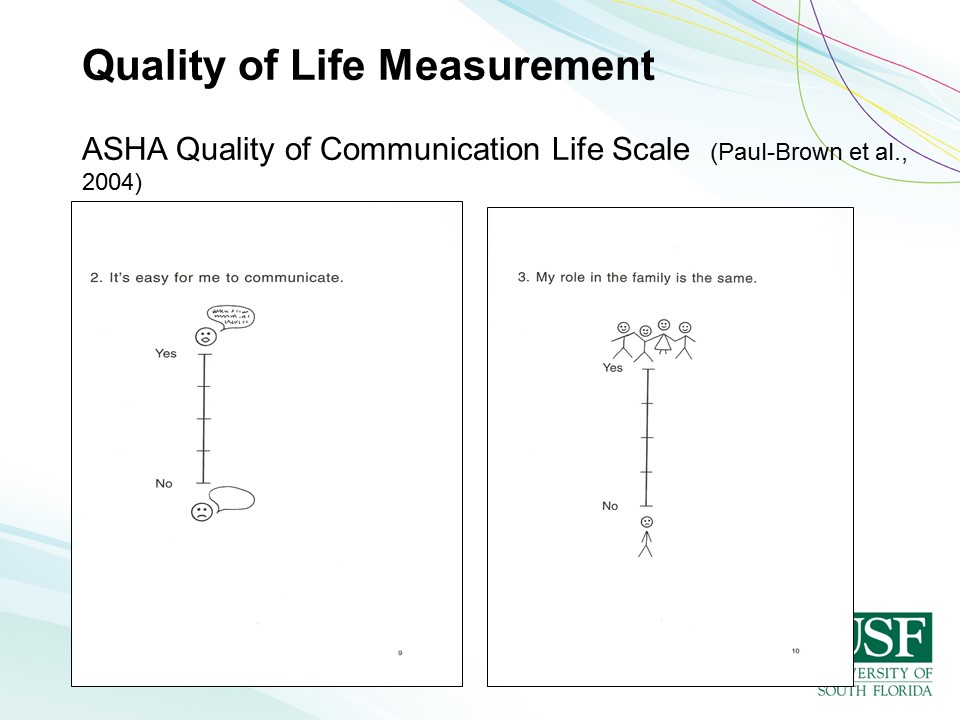
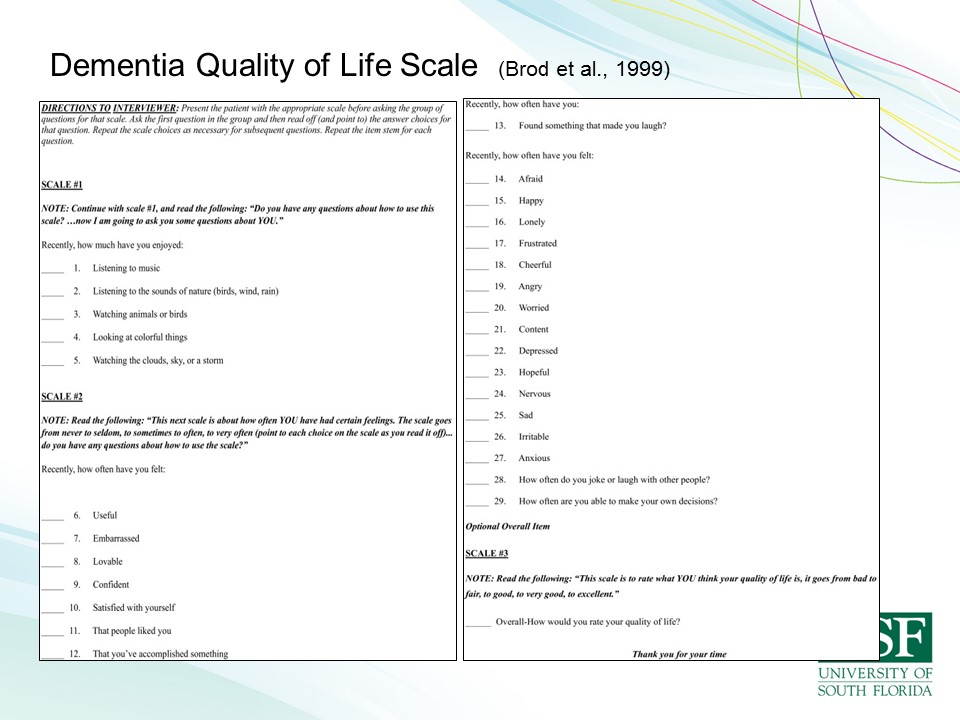
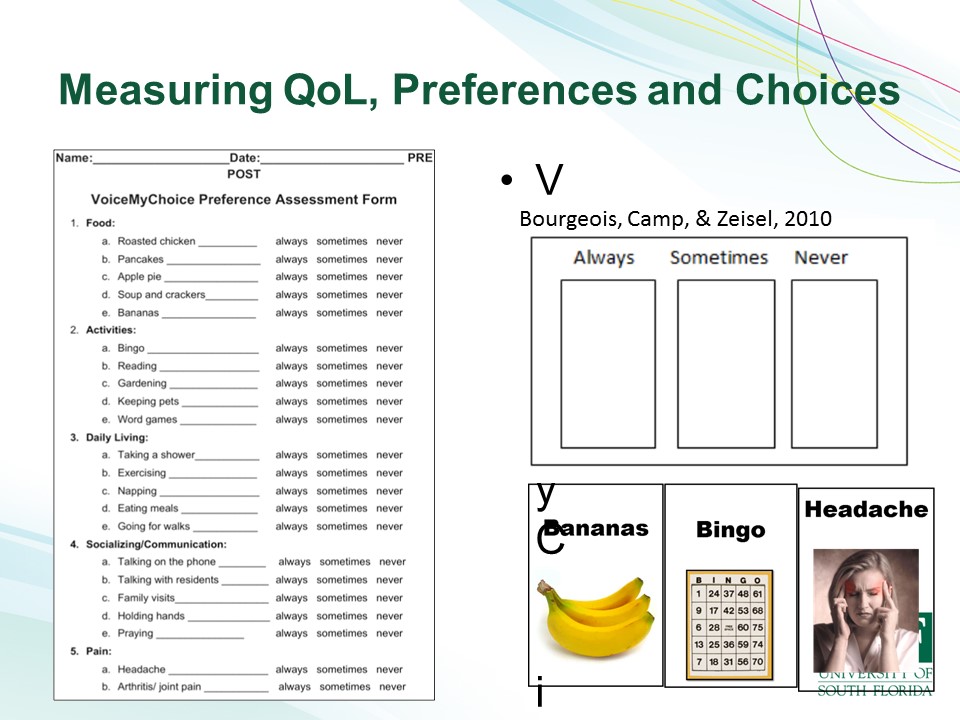
So there’s quality of life measures, there’s lots of quality of life measures.

[See the full video at: https://www.youtube.com/watch?v=1LCRrcxlrXE.
>> Nelly, could you help me of arrange some flowers for the tables this morning?
>> Yeah I can try it.
>> You can try it, fantastic. Let me get some bowls down.
>> And Marge just thoroughly enjoyed the activity. She’s been able to– well, do some of the things she’d done in former life, I suppose, such as drying the dishes or folding the serviettes, helping make beds even.
>> Hello Marge.
>> Hello Dia.
>> Do you like to help me clean the whiteboard?
>> I’m going to [inaudible]–
>> Oh thank you. I just called one of these, just one and you want like this. Can you this? It is beautiful. Beautiful, thank you Marge, did a great job.
> The environment is changing and interactive and offers opportunities for staff and residents to interact in a meaningful way.
We have to stop. I hope that entice you to go home and watch the whole thing and to think about the possibilities of incorporating meaningful activities and a different way of interacting with people with dementia.
Questions and Discussions
Audience Comment
That was a lovely presentation and it’s reminiscent of things I’ve been hearing for the last three days, which is looking at practice-based evidence, taking the evidence that we have, looking at practice-based evidence, thinking about quality of life in a different perspective. Not what I think it might be for you, but about what you think it might be for you. But the most telling thing that I’ve learned from your talk today and others is how you ask questions so that you ask the questions that get the information that you want to know that well, then help you create the treatment or the assessment. And I think that’s important in what you’ve said.
Thank you, yes. Yes and we need to ask the questions of the person with dementia. And I have another whole talk on decision making in dementia. We assume that people with dementia can’t make decisions at a certain point and they can’t, they don’t have opinions and that is not true. We have tools for– visual tools for helping them with that. And it’s remarkable what information you can gain from them when you give them the appropriate tools for communicating.
Audience Question
So you talked about one of the questions that you want to answer is how to reduce negative beliefs around memory loss. Have you thought about ways to that and in particular, mindfulness or meditation?
Yes, so thank you. Yes. So there are a lot of other approaches and things to do and mindfulness is one, doing caregiver support groups where you have people coming together and talking about these issues is also helpful. So in the groups that I run with the clients with memory loss and the– and those the other group with family members talking about the same issues, it’s very useful to see that their attitudes change when they see that other people are experiencing the same things. And when they see successes in other people and then they see oh, yes my person is doing it too and then so there needs to be a lot more of that kind of intervention to help people getting to realize that these things are effective and they’re good for them. So, yes.
Audience Question
Years ago at the Boston VA, on our aphasia neurobehavioral unit we had a woman with Alzheimer’s disease. And she, like a lot of people with Alzheimer’s, she couldn’t sit still. And she had been a house cleaner. So our nurses always practical, they got her a feather duster and yeah, you know, and a bucket and wet sponge and let her, clean the unit. It was the cleanest unit has ever been, cleaner than the janitors did and she was so happy and she felt like she was helping everybody.
Yes, yes. And so if you watch this video, there are multiple examples of people doing jobs. There is man in here who pushes a beverage cart and offers beverages to other residents. Would you like a drink? You know, their frequency of dehydration and related problems like delusions and whatever related to dehydration, totally gone now because this friendly man is walking around offering them beverages all the time. The major outcome of this implementation of this approach in this nursing home has been to reduce psychotropic medication use from at least 80% PRN in that facility to zero, zero. And so, I’m working to replicate this in the US and have those kinds of outcomes and a lot of other ones and some video that’s American English. So sometimes, the Australian English is hard for people to understand right away but there are many, many examples of other things here. These people make their own coffee. They have food tables where they’re selecting their own food. There’s a woman who washes the dishes. Somebody else to dries dishes. Residents make their own beds. They help with the cleaning and all manner of things so it’s home. It’s home. It’s meant to be home. And so incorporating all the things that you would do at home makes it home, and people have a reason to get up and they have their job. The lady that was changing the reality orientation board, she was a school teacher. What did she do her whole career, right? She had a board like that with her kids and they did morning time everyday. She didn’t need to be taught how to do that. It was a preserved behavior. She knows how to do that. And all of these skills and behaviors that people have, we are not taking it– we’re not pulling out, we’re not getting them to utilize those things. So, there is such potential for making quite a big difference in how we do it. But I think our profession needs to really reevaluate how we go about assessment intervention, goal writing and all about stuff so that we are hitting the right targets and measuring the right things. So we need to be measuring quality of life and making sure it’s a meaningful life for people. So, thank you.





