The following is a transcript of the presentation video, edited for clarity. Click the PDF icon to download the presentation slides.
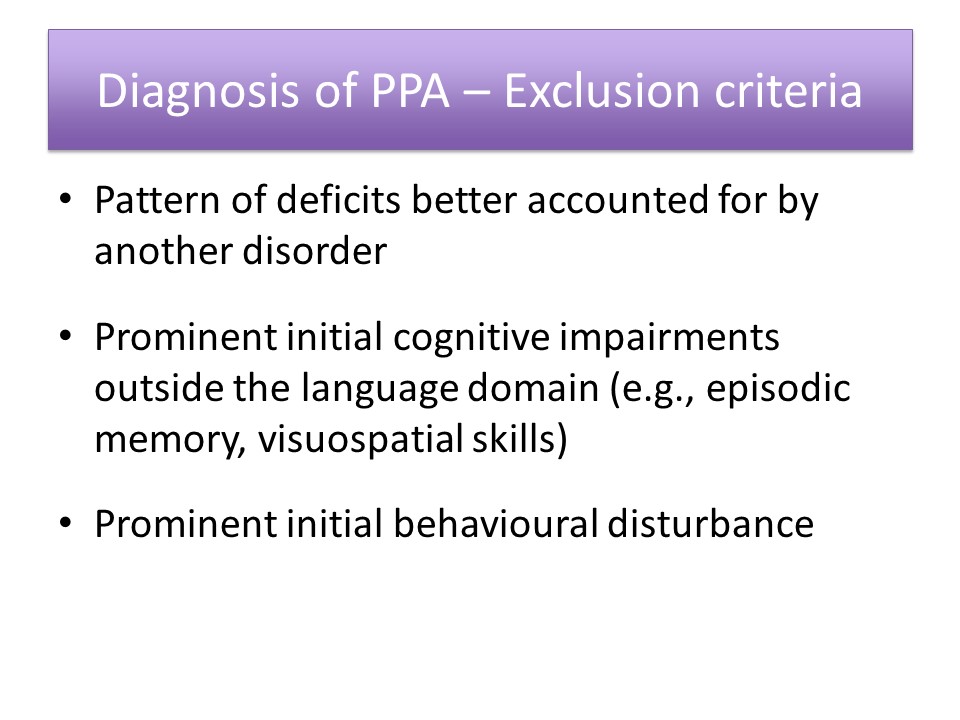
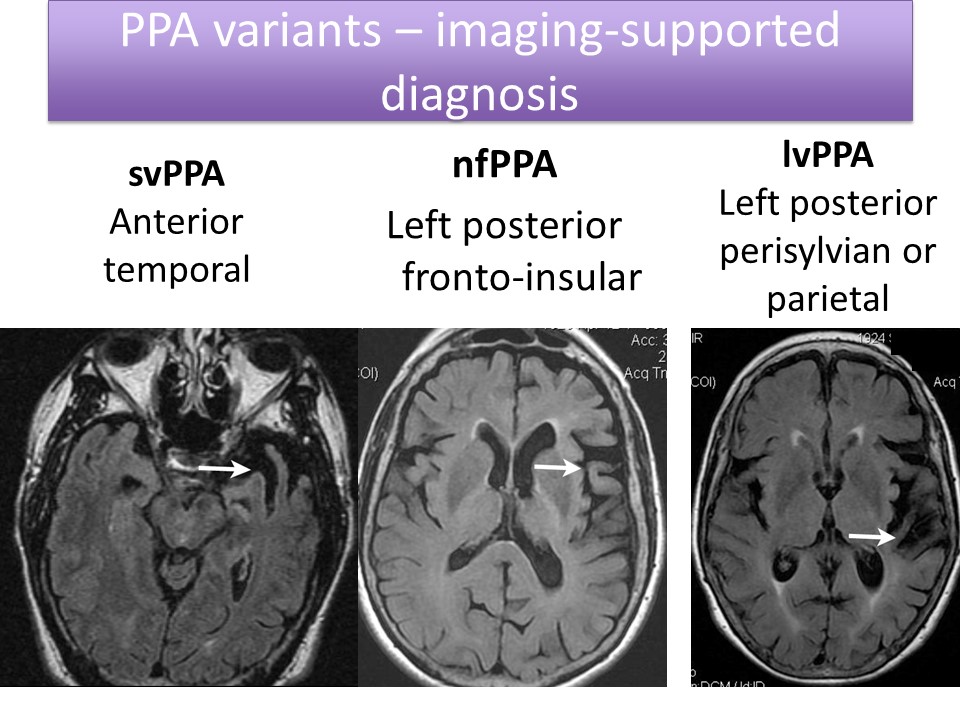
Diagnosis of PPA
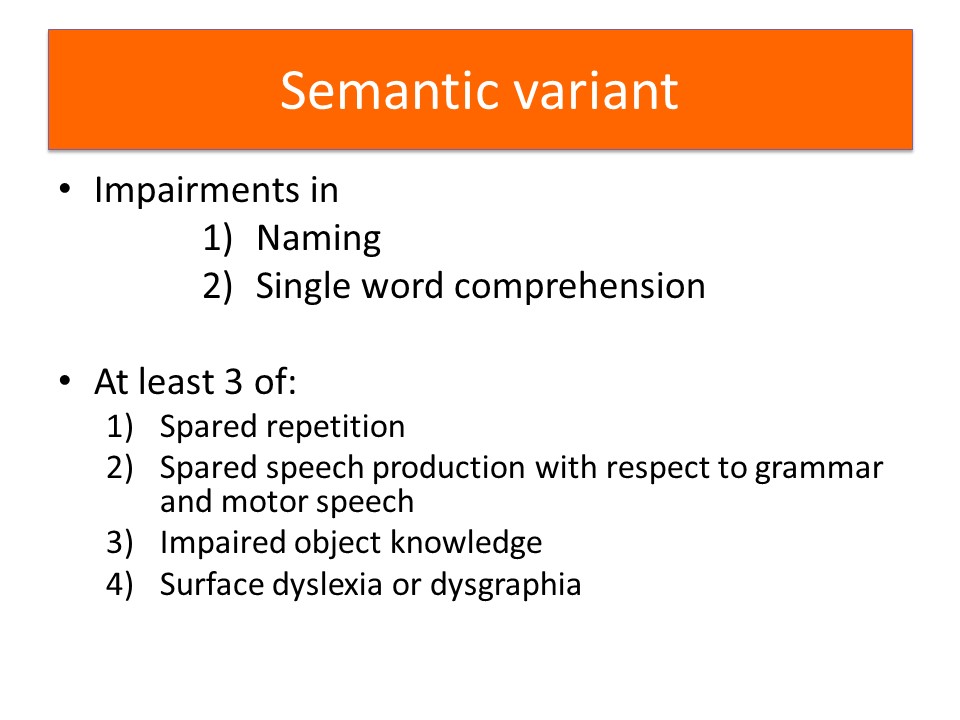
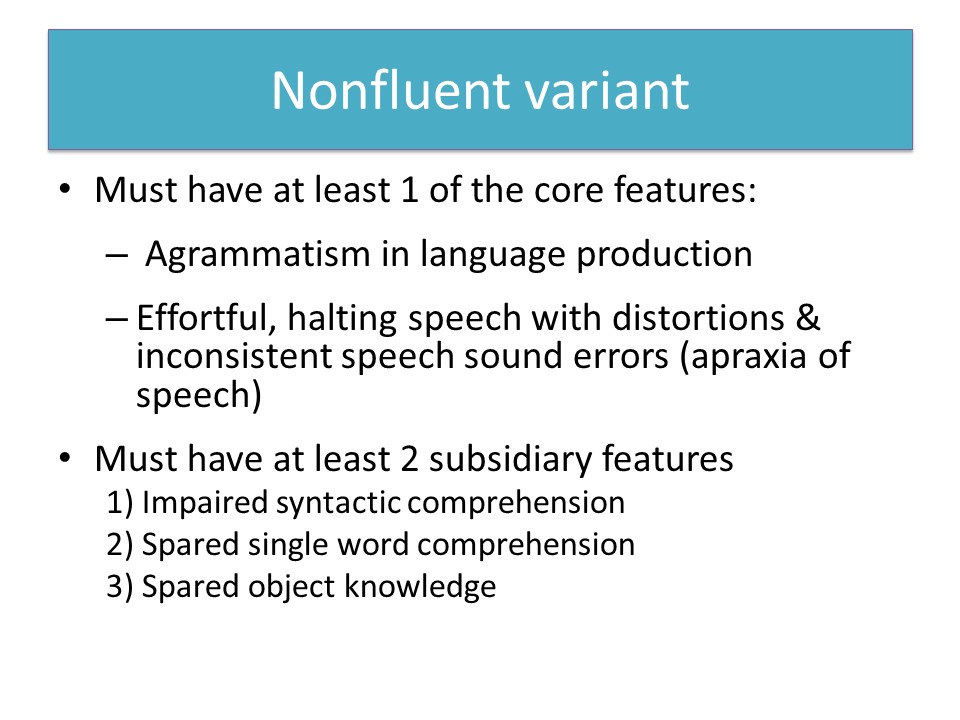
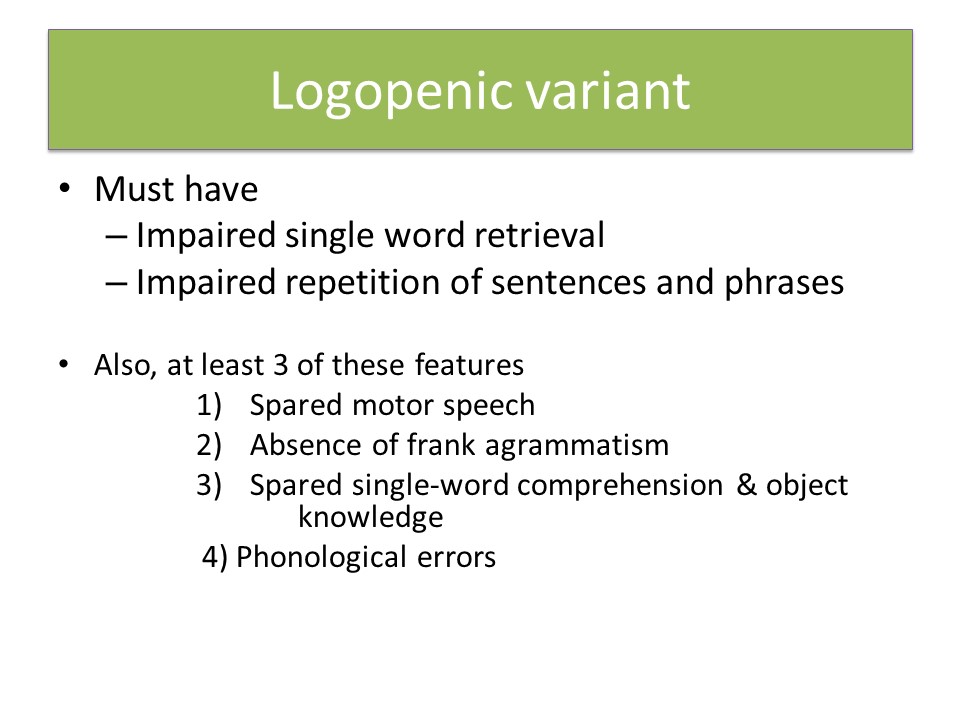
Description of Connected Speech in Each Variant
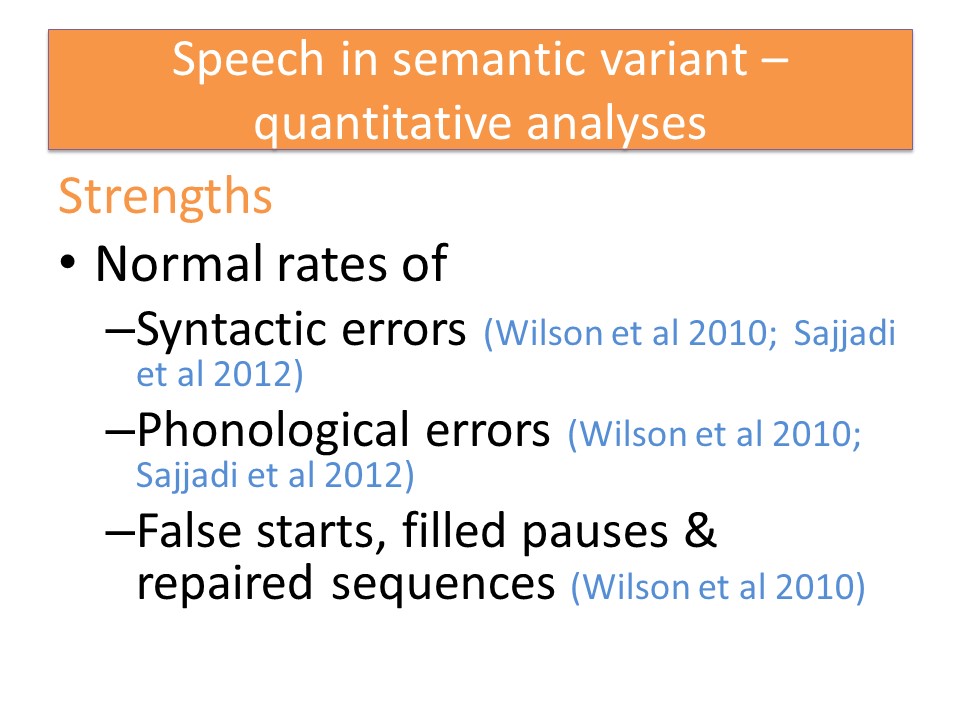
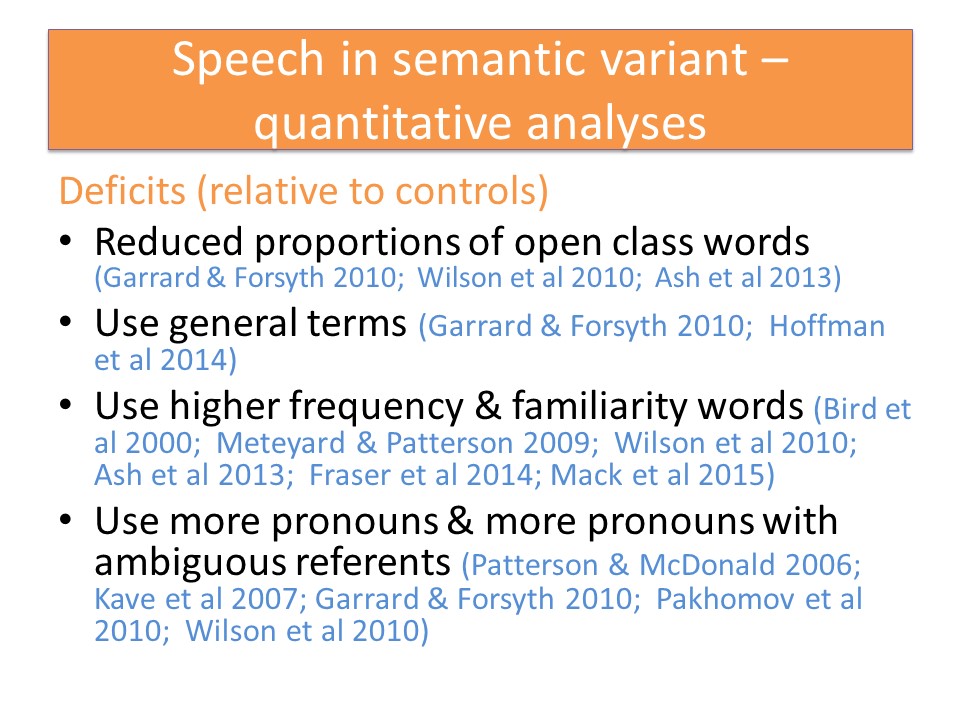
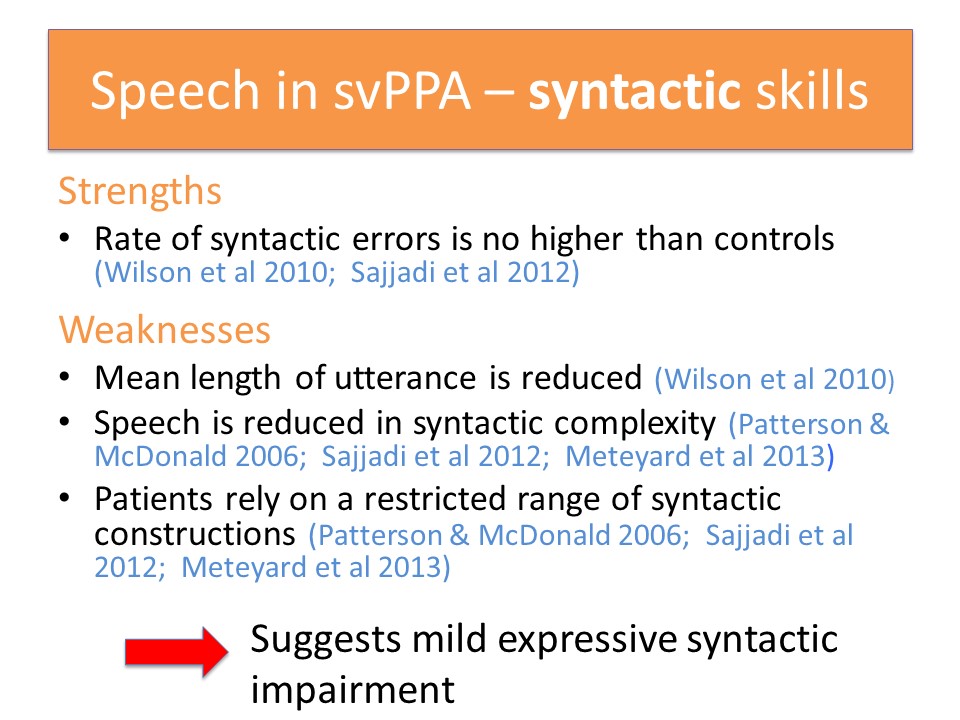
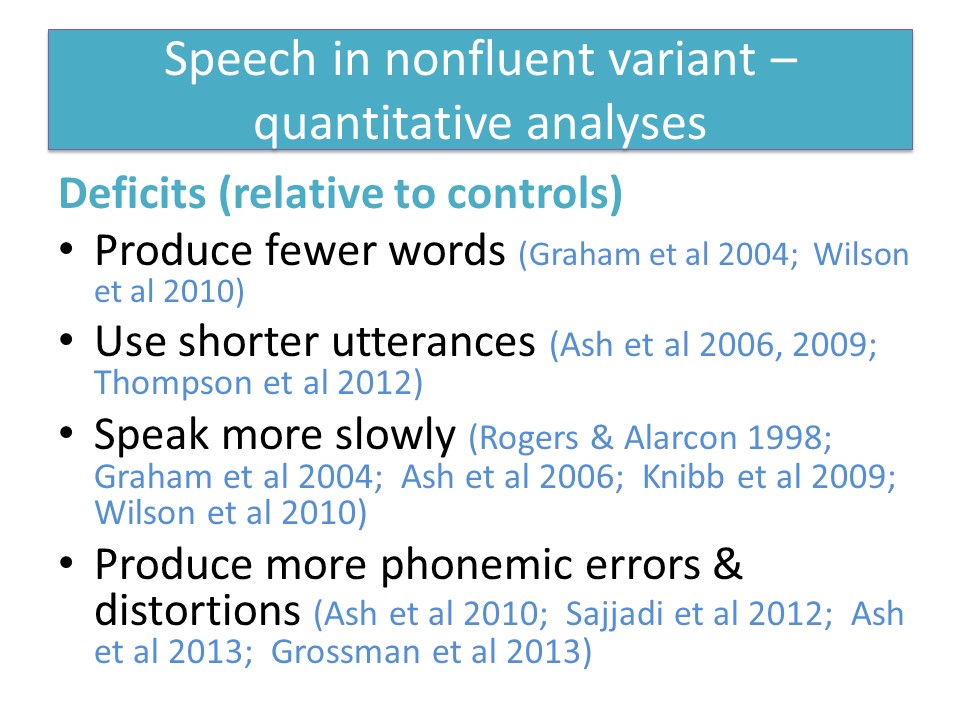
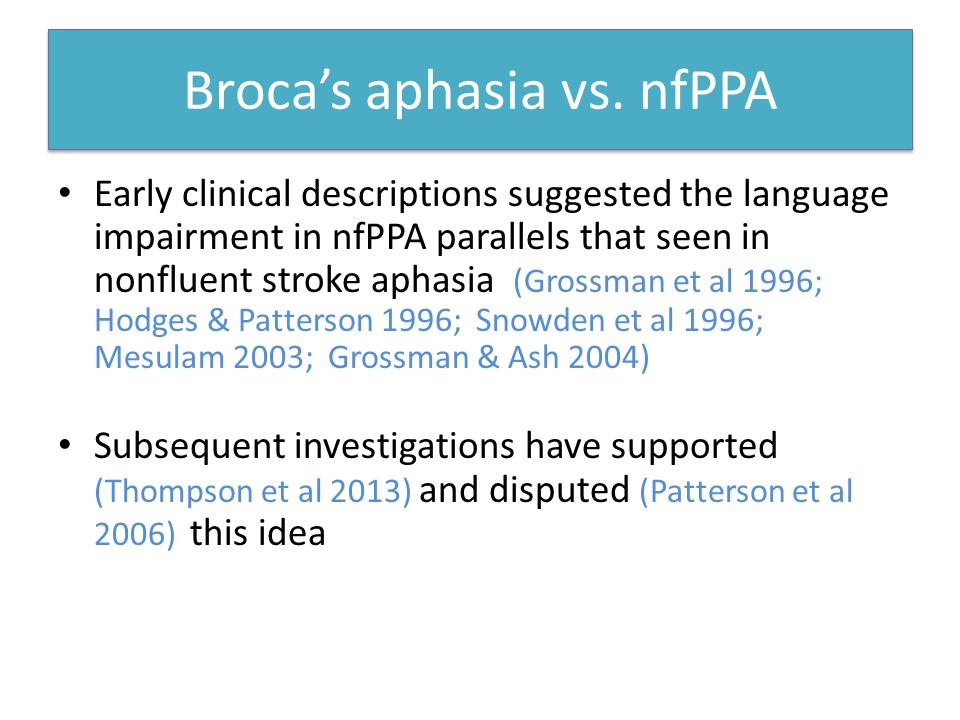
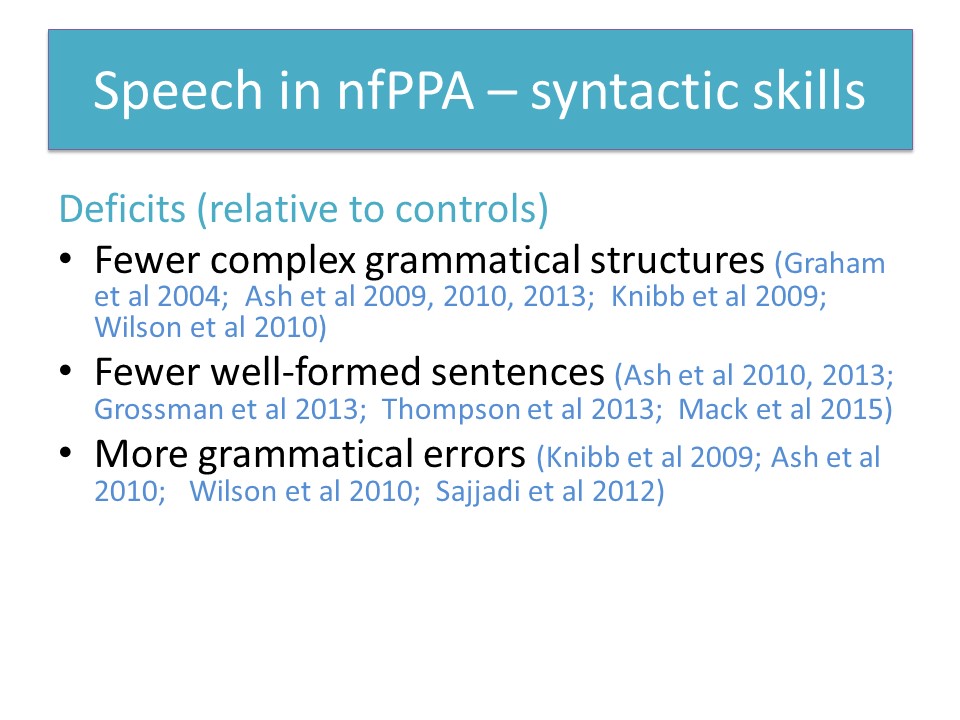
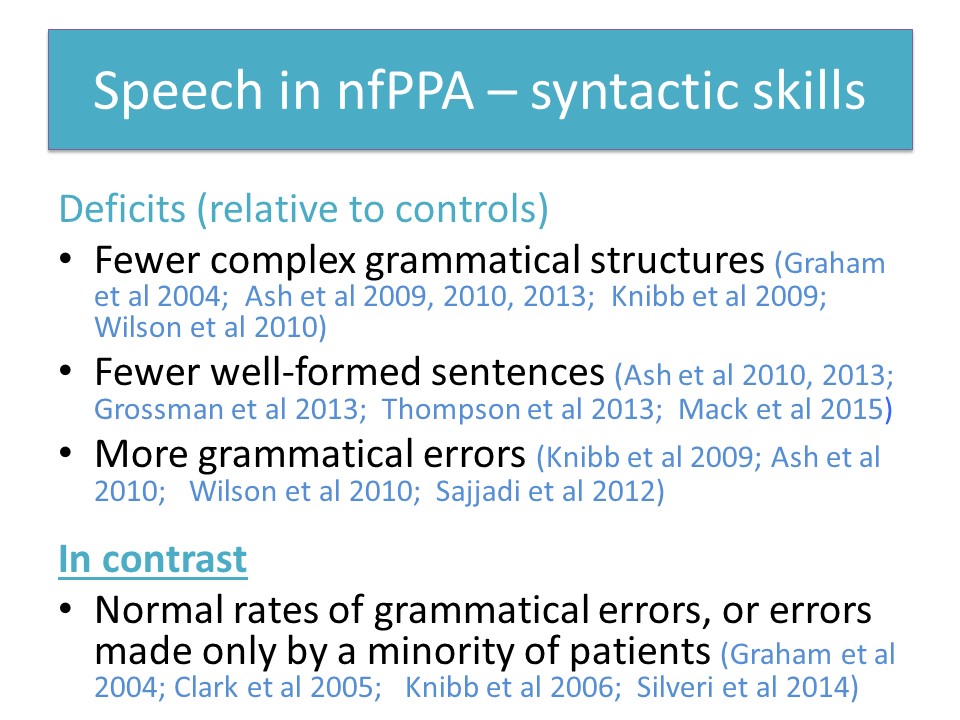
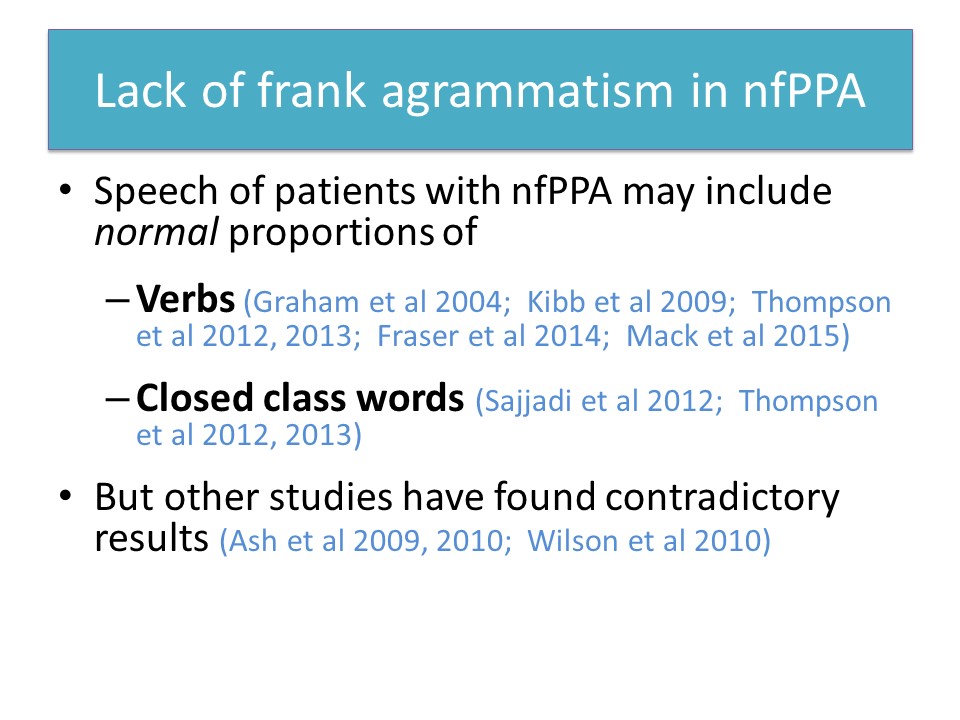
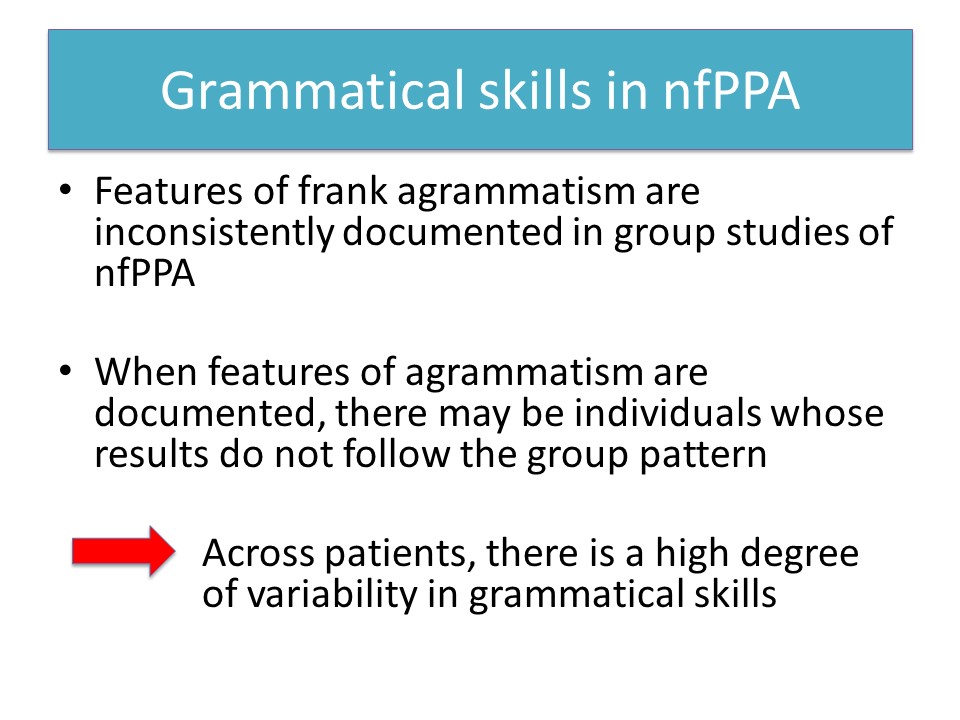
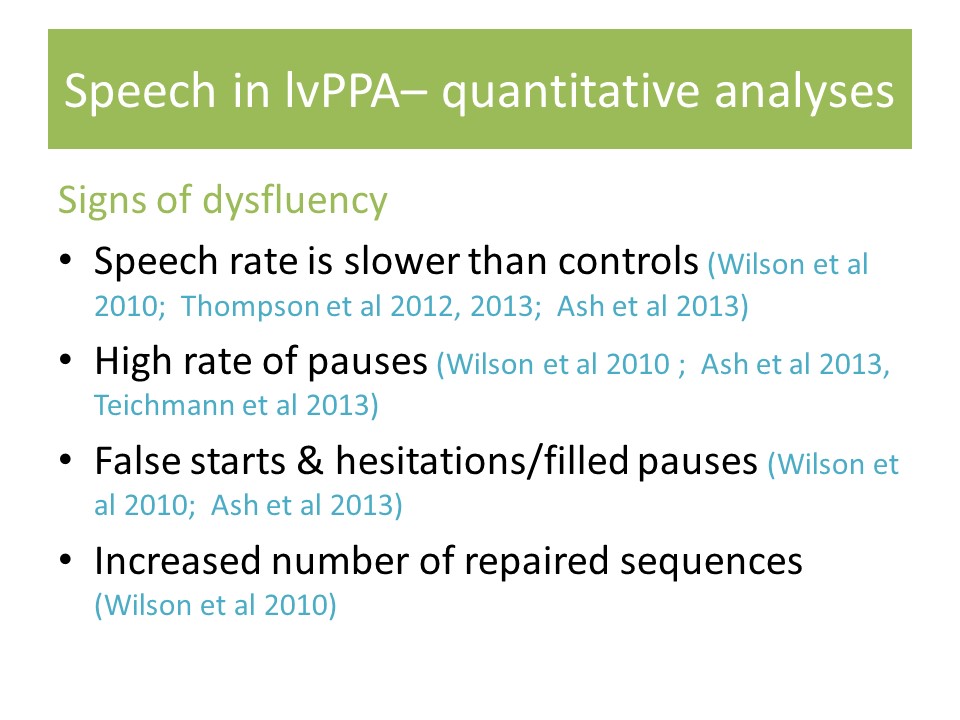
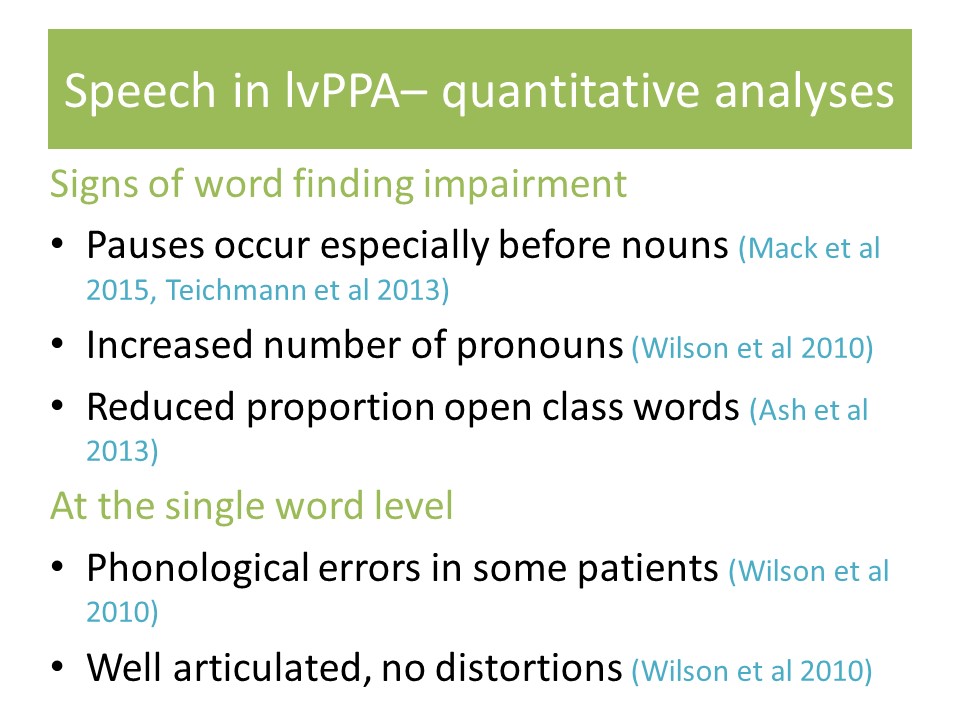
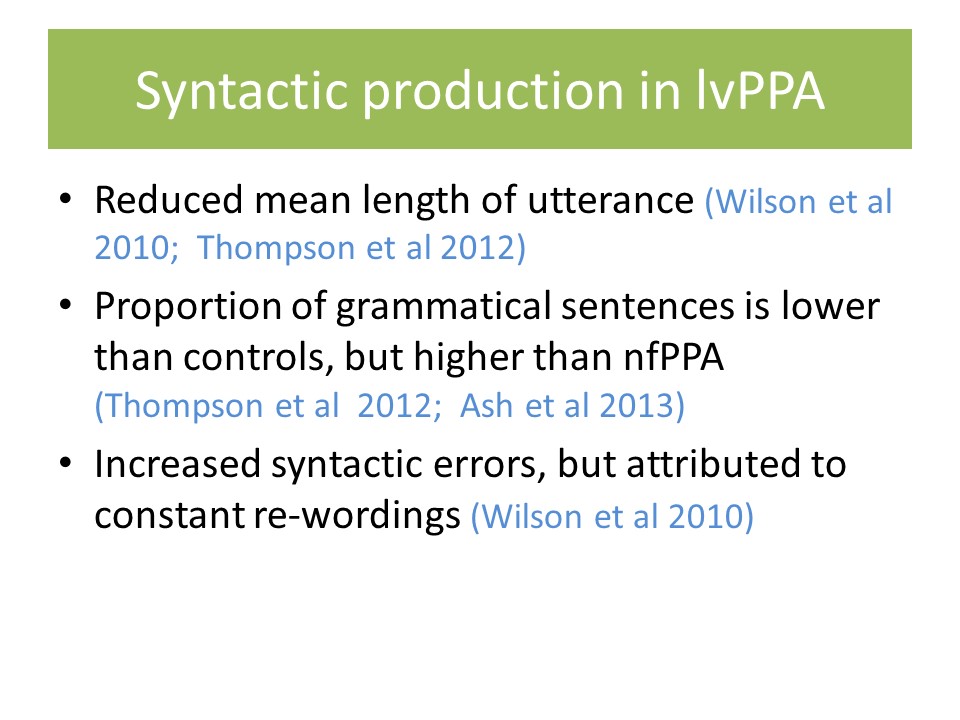
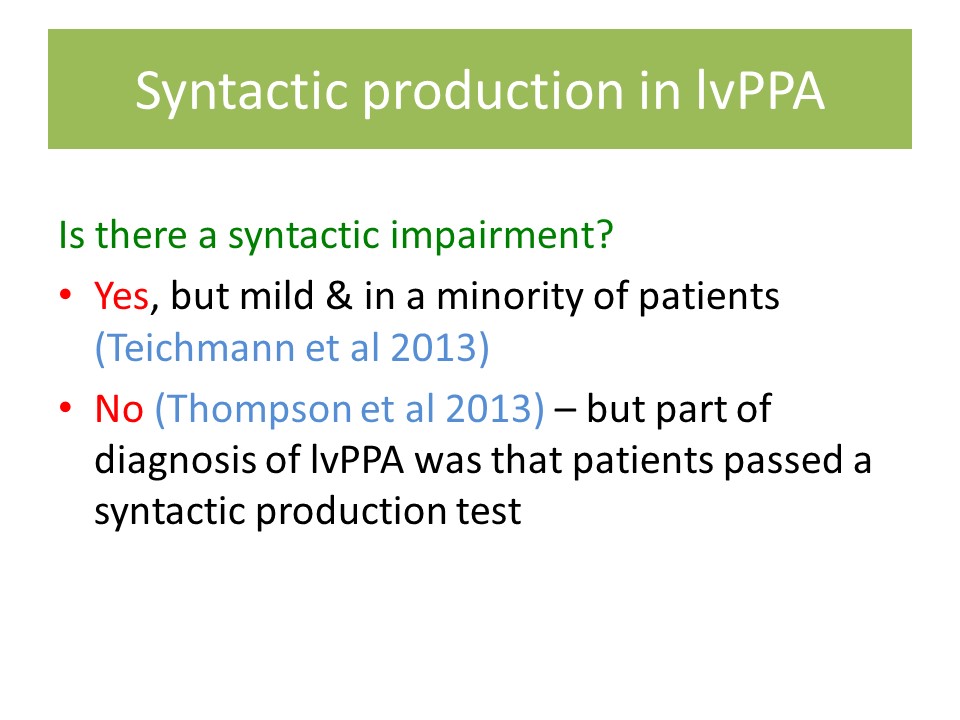
So now I’m going to describe connected speech in each variant, and I’m going to focus particularly on quantitative analyses that have been published in the literature.
Starting with the semantic variant it’s been shown that these patients have normal rates of syntactic errors, phonological errors, and false starts field pauses, and repaired sequences.
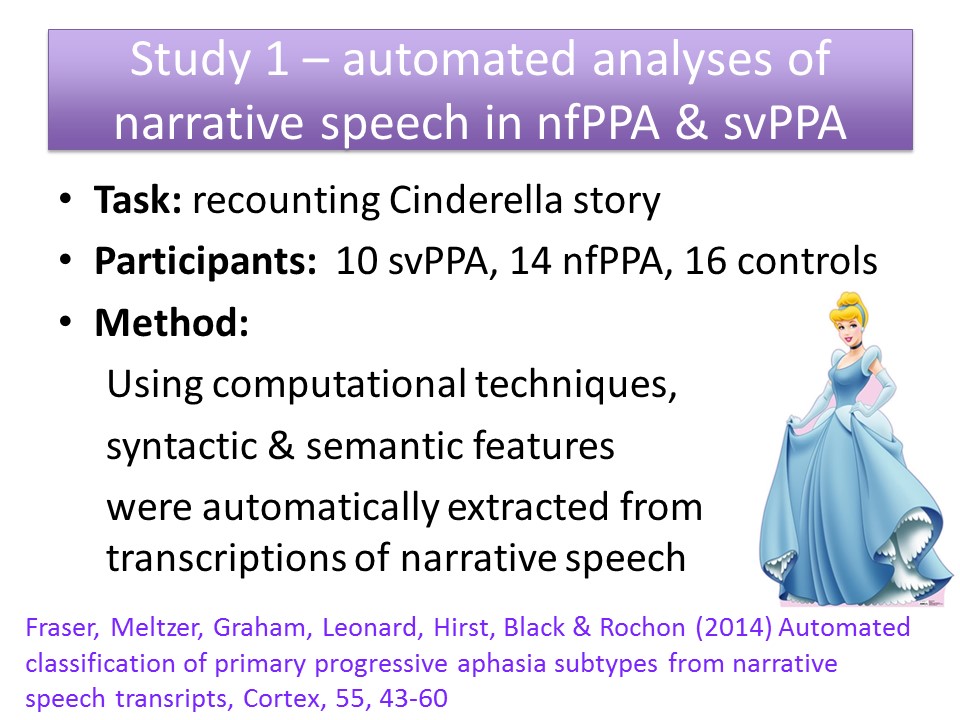
Study 1: Automated Analyses of Connected Speech in PPA
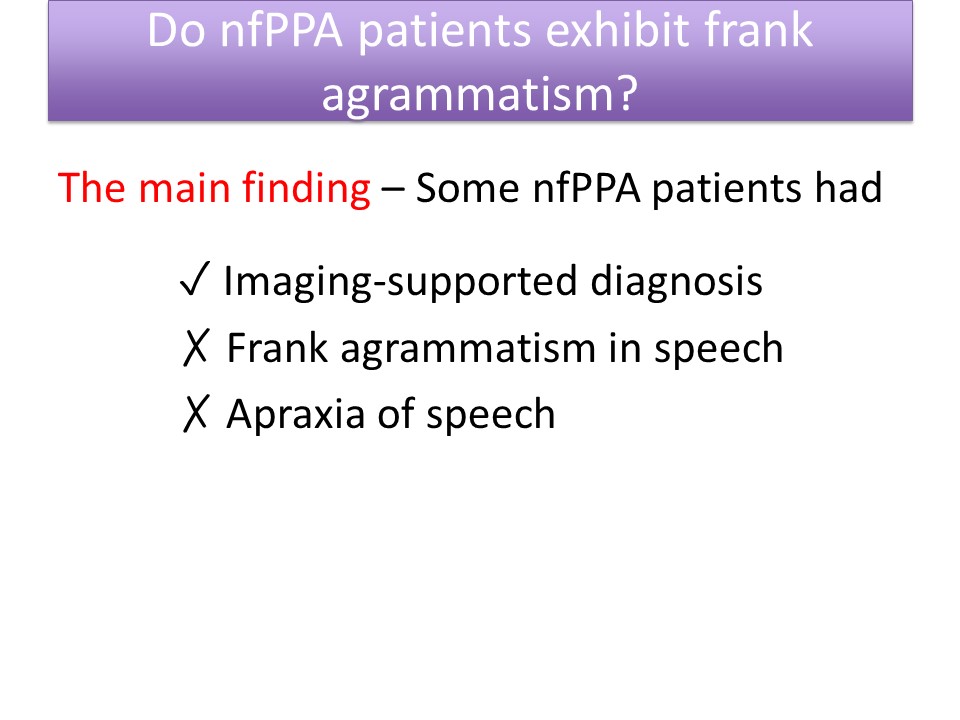
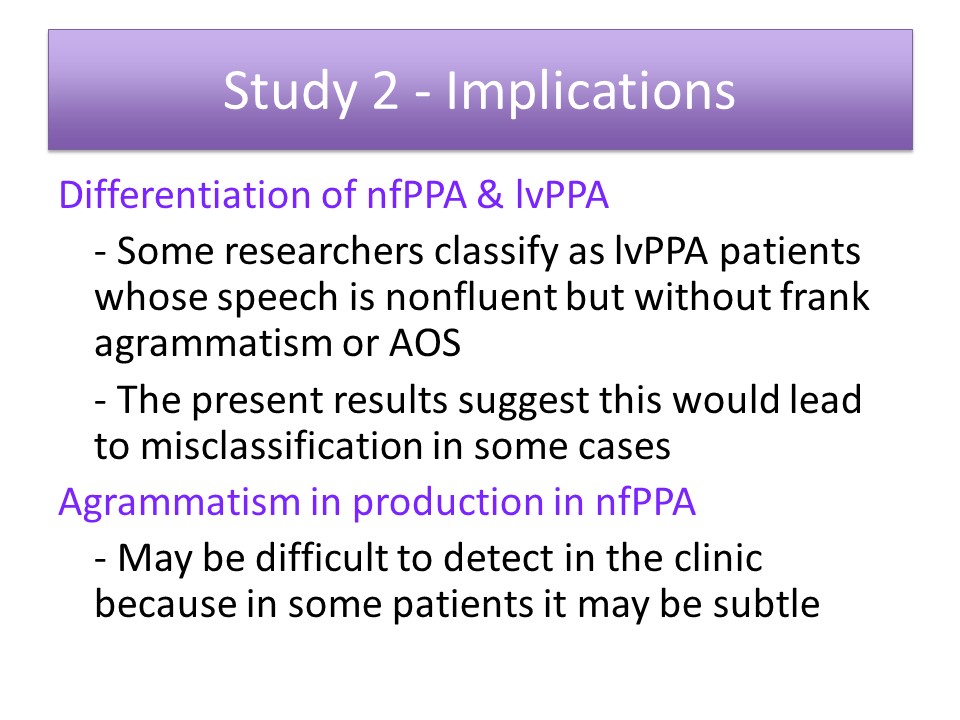
Study 2: Evaluation of Agrammatism in Nonfluent Variant PPA
Study 3: Agrammatism in Spoken vs. Written Production in nfPPA
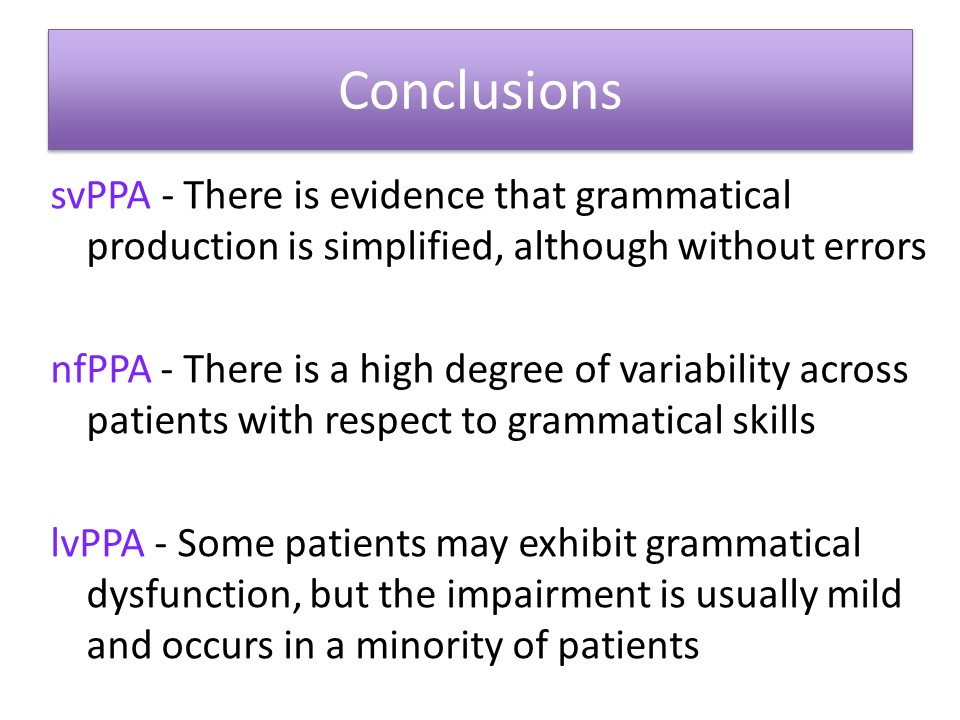
Final Comment & Conclusions
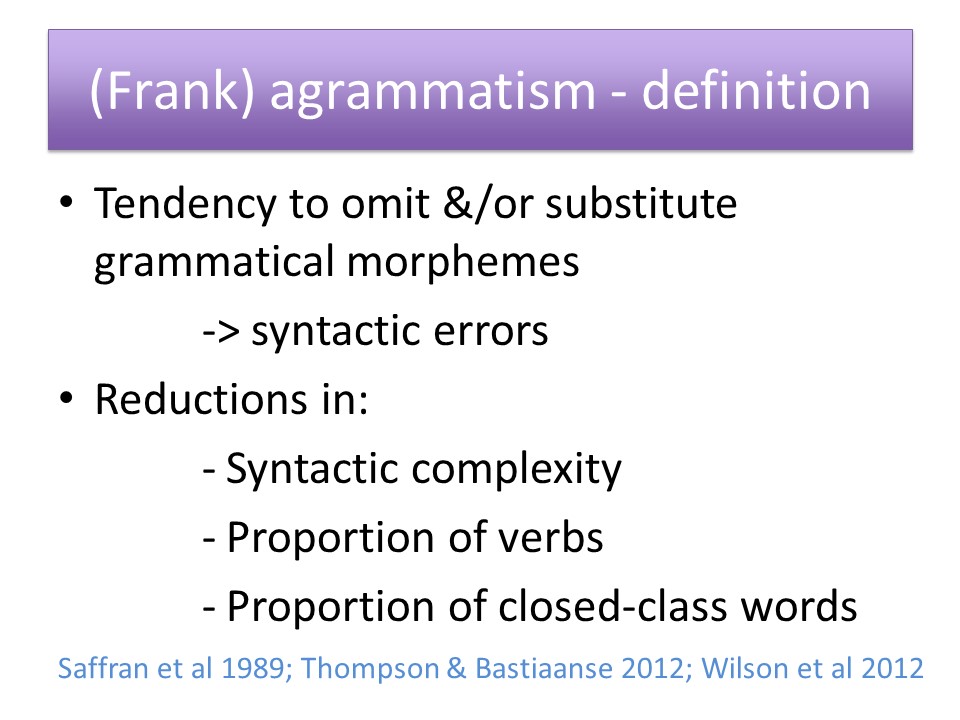
So I’m going to now just finish with one slide that’s got some final comments, and then I’ll finish the conclusions. Now, because I’ve noted that there’s variation in the literature with respect to how PPA patients are subtyped, it seems that we need better ways to systematically evaluate grammatical production. So most of us evaluate grammatical production by listening very carefully to patient speech, and I’m certainly not saying that we shouldn’t do that, but I looked for some more systematic methods of evaluating grammatical production.
So I’ve identified some assessments in the literature that may be useful. So first of all there’s the make a sentence test which is by Billette et al in their publication in Aphasiology they’ve included all of the stimuli for this test, so in this test patient is shown written words — so for example Emma baked pie party– and then the patient has to produce a spoken sentence and inflect the words. So then they correct answer here would be “Emma baked a pie for the party.”
Results from analyses done by Billette et al show that performance on their make a sentence test was strongly correlated with measures of patient spontaneous speech, especially production of grammatical errors and abandoned utterances. Billette et al compared performance on their test with performance on the Northwestern anagram test, which is by Weintraub et al. So that’s another test in which patients have to make sentences, but they just have to arrange words to make a sentence, they don’t have to speak the sentences in that test. Billette et al found that the make a sentence test was less prone to ceiling effects and therefore was better at picking up subtle early deficits.
There are also two rating scales that have been developed specifically to evaluate language impairments in primary progressive aphasia, and both of these scales provide ratings for severity of impairment in grammatical production and morphology.
Questions and Discussion
Audience Question
Hi, I’m Alyssa Lanzi from Duquesne University. I was wondering how a patient’s cognitive decline can affect their discourse measures that you’ve seen in your research.
Audience Question
I just would follow up. I think Alyssa’s question is a good one because perhaps we could turn it around and say “Do you think in the language domain there are some early indicators that widespread cognitive decline is about to, or is beginning to happen?
Audience Question
I’ve been wanting to ask someone like you just for a couple of days because now I’ve listened to about six hours on primary progressive aphasia. A prevalent symptom — language problem — in aphasia with stroke is perseveration, and I haven’t heard anybody talk about perseveration in primary progressive aphasia, and looking in the end, what you showed today of course when to set out, you looked at a heck of a lot of cookie thefts and so forth. So can you make any observations on that?
Audience Comment:
Audience Question
Were there any medication implications regarding your clients?
So the most of our patients are not being treated. So there just because there is, this no cure for progressive aphasia. So you know some of them are on various medications, but it’s actually something that we deliberately adopted a policy of ignoring, or at least we could, we can’t control for this in our research. It’s not so much that we ignore it but we can’t control for this because certainly for the research that were doing. We can’t ask people to abstain from medications, it would be unethical. So for us it may be creating noise in our data, but it’s just something we have to tolerate.
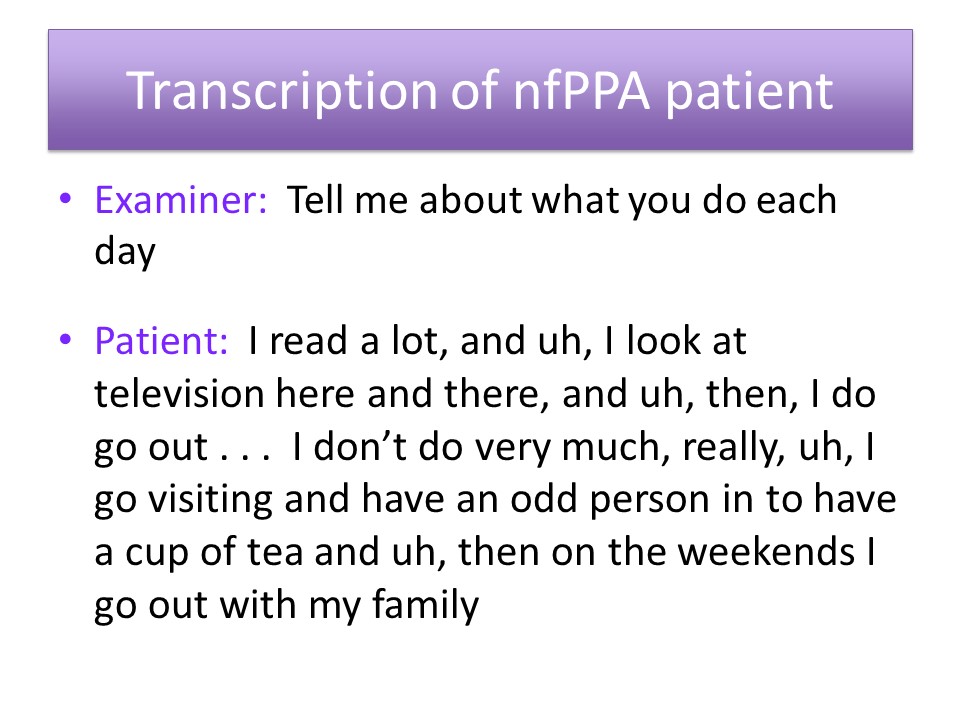
Something I found fascinating is to see all these MLU reduction in patients for progressive aphasia, but in terms of eliciting a response but when it comes to echolalia the syntax is perfectly intact. It is surprising. I guess everybody heard so the ideas in echolalia wise, it’s surprising the syntax is completely intact, and it’s surprising to me too with some of the more severe non-fluent patients that I’ve seen that who are was still producing syntactically correct utterances. It’s you know, it’s amazing how this holds up obviously some people are agrammatic you know, right from early on in the illness, but some of them even the people without motor speech impairment are still able to produce syntactically correct utterances, even when they’ve had the disease for a while and their speech is pretty non-fluent.





