Few can argue with the evidence that supports better outcomes, greater satisfaction, and more cost-effective care as a result of interprofessional collaborative practice (IPP). To prepare students who will soon enter IPP work environments in health care and educational settings, interprofessional education (IPE) is required. From our experiences at MGH Institute of Health Professions, we found that implementing a meaningful IPE focus is a long-term process. Although many things remain a “work in progress,” we made great strides in providing our students with both academic and practical training to become effective members of interprofessional teams. This article focuses on our journey and the lessons learned along the way. Recognizing that “one size does not fit all,” we share part of our story in hopes of offering some guidance to any program that is attempting to begin constructing or enhancing their own IPE experiences.
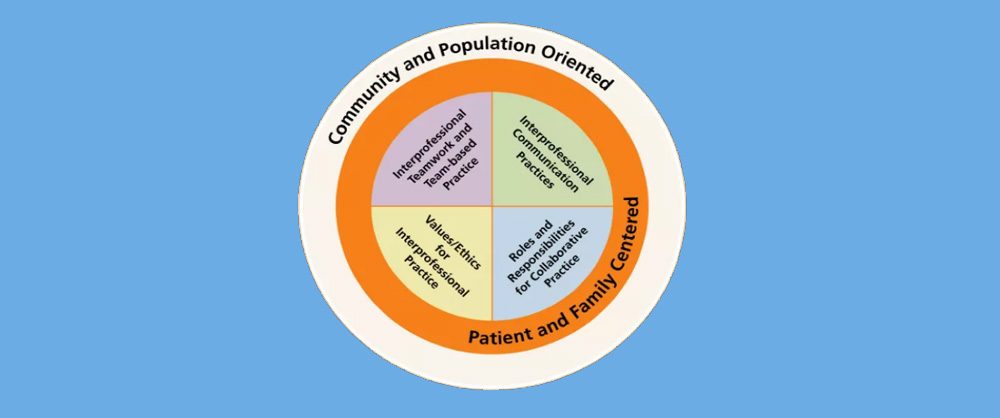
Since its inception in 1977, the MGH Institute of Health Professions has confirmed its commitment to teaching students to become evidence-based clinicians who are high- performing members of interprofessional teams. Early IPE efforts came in the form of interspersed classes open to multiple disciplines and thoughtful seminars exploring topics of mutual interest. Fast forward to 2011, when the Institute faculty embraced a more comprehensive interprofessional vision, making our philosophy explicit and fostering the development of a wider array of courses and activities to make interprofessional values more integral for all students. This process resulted in the creation of IMPACT Practice®, an overarching conceptual framework for IPE that serves as the context for learning across all of our programs. Creation of this framework required serious compromises, added resources, and a dedicated collaborative effort. The foundation of the framework is built on the identification of six core competencies that reflect the knowledge, skills, and attitudes required for all Institute graduates to provide contemporary care in our complex health/education systems and communities (see Figure 1). These competencies subsume the Interprofessional Education Collaborative (IPEC) competencies (see Figure 2) and complement uniprofessional competencies for all disciplines.
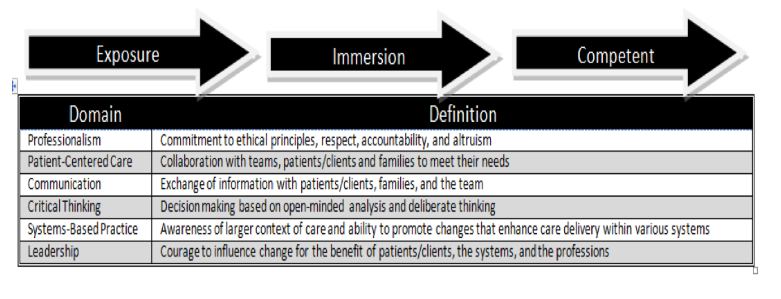
Figure 1: MGH Institute Common Core Competencies Across Six Domains
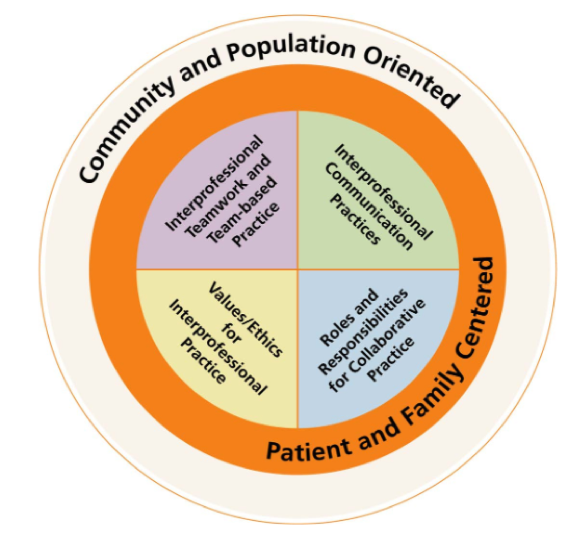
Figure 2: Interprofessional Education Collaborative (IPEC) Competencies
Retrieved from http://jdc.jefferson.edu/cgi/viewcontent.cgi?article=1052&context=jcipeconference
Source: Interprofessional Education Collaborative Expert Panel. (2011). Core competencies for interprofessional collaborative practice: Report of an expert panel. Washington, D.C.: Interprofessional Education Collaborative. Retrieved from http://www.aacn.nche.edu/education-resources/ipecreport.pdf
Meeting the Competencies
IMPACT Practice® (hereafter, “IMPACT”) is infused within curricula for the graduate programs in communication sciences and disorders (CSD), nursing, occupational therapy (OT), physical therapy (PT), and physician assistants. It includes several required and elective opportunities that are integrated throughout the programs.
Courses
All students take three sequential one-credit IMPACT courses, in which they work together on five- to six-person interprofessional teams with a mentor, learning the components of IPP and ethics while participating in community and simulation activities. The CSD program also offers multiple core and elective courses that are open to all students at the Institute—with content relevant to multiple disciplines (i.e., augmentative and alternative communication [AAC], pediatric feeding and swallowing, autism spectrum disorders, counseling, genetics, traumatic brain injury [TBI], early intervention)—providing opportunities for interprofessional perspectives and discussion.
Activities and Clinical Experiences
Community Impact Day. During their first fall semester, 350 entering students from the five programs, working in their IMPACT teams, partner with a faculty member as they set out into the neighboring community for one day to perform a wide variety of service activities (e.g., prepare meals for vulnerable elderly individuals, educate parents about early literacy, exercise with public school students). Returning to campus, the teams engage in reflective activities that are tied to the IPEC competencies of teamwork and values. These topics are later expanded upon in their IMPACT courses.
Common Reading. A relevant patient-centered narrative (e.g., this year, it was Lisa Genova’s book Inside the O’Briens, 2015, Simon & Schuster) is assigned prior to arriving on campus for the first day of classes and is discussed in discipline-specific cohorts during orientation, with themes later woven into the first IMPACT course.
Schwartz Center Educational Rounds. In 2003, the Institute became the first graduate school in the country to initiate “Difficult Conversations: Schwartz Center Educational Rounds,” an interprofessional forum that occurs four times a year. The forum features student presenters and discussions about difficult emotional and social issues that arise in caring for patients (e.g., “Caring for the Perpetrators of Trauma” and “Engaging LGBT Elders”).
Interprofessional Rounds Lecture. At this annual event, second-year students across programs come together to hear successful examples of how clinical teams collaborate to provide patient-centered care (e.g., “In Our Own Voice,” presented by the National Alliance on Mental Health Illness, and “The Journey of a Patient with Dementia, His Family, and Team of Clinicians.”)
Infant Development Day. Interprofessional student teams actively observe infants and toddlers, documenting developmental milestones while children interact with interprofessional faculty members. The session is followed by a debriefing that highlights a holistic team approach to child development.
Interprofessional Clinical Experience (IPCE). The Institute partners with Massachusetts General Hospital to offer the IPCE for our students across all programs. Paired in interprofessional dyads, the students participate in two half-day active observation experiences on Interprofessional Dedicated Education Units within the hospital. Led by staff nurses and therapists who have been trained as interprofessional practice instructors, IPEC competencies are reinforced within rich debriefing sessions.
International Innovations Project. Institute students can apply to become participants on international (Danish, Finnish, and American) interprofessional teams, collaborating for 5 weeks during the summer break to create innovative solutions to current community problems.
Crimson Care Collaborative. A nurse practitioner and a physician assistant from the Institute work together with Harvard Medical School students in an interprofessional primary care setting for patients who have little or no insurance. Opportunities are being explored for CSD and other Institute students to participate in this student-led clinic.
Interprofessional Clinical Center. Our long-standing Speech, Language and Literacy Center is being modified to become an interprofessional clinical center, merging with the OT and PT clinical centers.
Lessons Learned
It has not always been smooth sailing in our journey to develop IPE experiences. We have started and stopped various endeavors, modified currently existing ones, abandoned impressive but unsustainable ventures, and learned much along the way. In the list below, we share several takeaways from the creation of these opportunities and an evaluation of the modifications that followed.
- Just start! Create a pilot project, even if it’s something small.
- Have a clear mission that provides guiding principles. The characteristics of each institution will determine the scope of what can be accomplished; the activities and clinical experiences detailed above work for our particular location, programs, resources, and level of commitment. Needs, priorities, and principles may differ from one organization to the next, depending on where you are.
- Leadership matters. A small group—one with vision and the authority to carry out the initiatives—needs to champion these efforts.
- Get buy-in. Explicit messaging that highlights the value of IPE needs to be continually emphasized with faculty, students, administration, and clinical partners.
- There will be sacrifices (but it’s worth it). It will take some student credit-hour shifting, curriculum modifications, changing of faculty workloads, and, perhaps, shuffling of class times. Although these tasks may be challenging, they are essential for making IPE happen.
- Train faculty members in IPE. Faculty members need training. Ongoing faculty development opportunities need to be established to help faculty members understand how to teach in this model.
- Make friends. By breaking down our discipline-specific silos, we can engage in collaborative initiatives where everyone is on equal footing. Do your best to ensure that one discipline does not dominate.
- Remember: IPE does not occur in a vacuum. Infuse activities and an interprofessional attitude throughout the curriculum. Perhaps an across-program syllabus review is a good place to begin.
- Make it part of the curriculum, not an add-on. Students have to see IPE as integral to their learning—not as “extra work.”
- Develop clinical partners. Make the experiences about practice; IPE is relevant only if it is applied to IPP, so seek out partnerships that will provide a connection to clinical education.
- Make it sustainable. All experiences must be cost-effective, efficacious, and efficiently run so that all students across programs can benefit. Always aim to balance quality with sustainability.
- Question it and study it. View this as a Scholarship of Teaching and Learning (SoTL) opportunity. Question all assumptions, obtain feedback, collect data, and be prepared and willing to make even major modifications.
- Students really want this. And they need it.
Regardless of the size of your institution, budgetary constraints, number of students, array of programs in your college/school, or number of current clinical affiliates, some form of IPE can be implemented. Whether it’s large scale or small scale, or somewhere in between, efforts to include IPE in CSD programs are necessary to ensure that the next generation is prepared to be impactful members of interprofessional teams in health care and education.
Resources
Interprofessional Education/Interprofessional Practice (IPE/IPP) webpages
Interprofessional Education/Interprofessional Practice Resources